Disco Ball! In The Sac
Written by: Dr. Jeffrey Chan
Edited by: Dr. Joann Hsu
Case:
22-year-old male presenting with one month of bilateral testicular pain with acute worsening over the past three days. Pain worsens when lifting heavy objects or bending down. He is five months status post right-sided orchiectomy for right cryptorchidism. He endorses mild discomfort and swelling below the surgical incision site, without overlying skin changes or rashes. Denies urinary complaints, including dysuria, hematuria, anuria, or penile discharge. No constitutional symptoms such as fever, headache, weight loss, nausea, or vomiting.
Vitals:
BP 131/72, Pulse 67, RR 16, SpO₂ 98% on RA, Temp 36.8 ºC
Physical exam:
Afebrile, well-appearing. Right inguinal incision with mild swelling and tenderness, without evisceration or dehiscence. Right scrotum empty. Left testis descended with vertical lie and intact cremasteric reflex. No swelling, tenderness, mass, or hernia. Otherwise unremarkable.
Lab results:
Urinalysis w/ reflex culture – Negative nitrite, negative leukocyte esterase, WBC <1, RBC negative, bacteria negative
Gonorrhea/Chlamydia – Negative
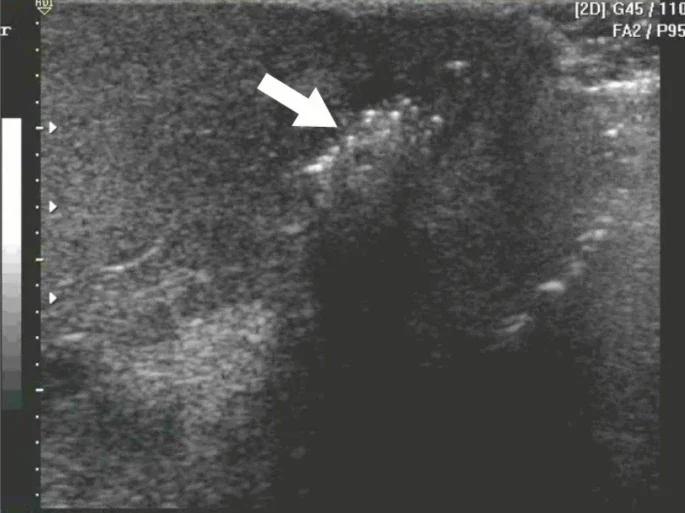
POCUS images of the left testicle:
Findings of bedside ultrasound:
Absent right testis (not pictured)
Multiple punctate, non-shadowing, uniformly sized, hyperechoic foci measuring 1–2 mm within the left testis.
No testicular mass noted. No anechoic fluid collection around the left testis concerning for hydrocele. No other significant findings.
Diagnosis/Finding: Left testicular microlithiasis.
Testicular microlithiasis (TM) is a condition of unknown etiology in which small clusters of calcium form in the testicle. It is most often detected incidentally on scrotal ultrasound.
Studies suggest an association with testicular germ cell tumors (TGCT) and intratubular germ cell neoplasia (IGCN), though causality has not been established.
Although the exact reasons are unclear, an association between IGCN and testicular microlithiasis has been noted. Up to 50% of patients with IGCN have been found to develop testicular tumors within 5 years.
The prevalence rate of TM in asymptomatic men aged 18–35 years, based on two ultrasound-based studies published in the Journal of Urology (2001 and 2008), is reported as 5.6%. In the pediatric population, the rate ranges from 2% to 4.2%.
Similar appearing pathology
The appearance of the hyperechoic punctate lesions may initially raise concern for air.
Reminder: air appears as hyperechoic punctate lesions on ultrasound with shadowing behind it. Think: bowel gas, necrotizing fascitis
However, testicular microlithiasis does not exhibit shadowing and as mentioned above, this is often an incidental finding that is not associated with any concerning acute symptoms.
Here is an example of air in the scrotum, concerning for Fournier’s Gangrene. You would expect clinical symptoms concerning for necrotizing infection such as pain, foul smelling discharge, necrotic tissue, fever.
Management:
The current consensus for management is self-examination, annual ultrasound until age 55, and clinical follow-up for those with genitourinary symptoms or additional risk factors (e.g., history of cryptorchidism, infertility, testicular atrophy, or family history of testicular cancer). No surveillance is advised for isolated TM in otherwise healthy individuals.
In asymptomatic men without additional risk factors, the absolute risk of developing testicular cancer is low. For symptomatic men or patients with additional risk factors, urology and surgical follow-up are strongly recommended.
This patient was referred to urology for testicular microlithiasis due to his history of cryptorchidism, and to surgery for post-orchiectomy scrotal pain follow-up.
Happy scanning!
References
https://www.sciencedirect.com/science/article/abs/pii/S1078143903001777
https://link.springer.com/article/10.1007/s11739-025-03864-z
Janzen, D. L., Mathieson, J. R., Marsh, J. I., Cooperberg, P. L., Del Rio, P., Golding, R. H., & Rifkin, M. D. (1992). Testicular microlithiasis: sonographic and clinical features. American Journal of Roentgenology, 158(5), 1057–1060.
Peterson, A. C., Bauman, J. M., Light, D. E., McMann, L. P., & Costabile, R. A. (2001). The prevalence of testicular microlithiasis in an asymptomatic population of men 18 to 35 years old. The Journal of Urology, 166(6), 2061–2064.
DeCastro, B. J., Peterson, A. C., & Costabile, R. A. (2008). A 5-year follow-up study of asymptomatic men with testicular microlithiasis. The Journal of Urology, 179(4), 1420–1423.
Kim, B., Winter, T. C., & Ryu, J. (2003). Testicular microlithiasis: clinical significance and review of the literature. European Radiology, 13(12), 2567–2576.
Richenberg, J., & Brejt, N. (2012). Testicular microlithiasis: is there a need for surveillance in the absence of other risk factors?. European Radiology, 22(11), 2540–2546