Go with the (color)flow!
Written by: Dr. Justin Varias
Edited by: Dr. Joann Hsu
Case:
Patient is an 83 yo F with PMH of HTN, HLD, DM, CAD s/p PCI on 9/26/25, presenting to the ED with concerns of swelling to the right wrist where patient had radial access for her LHC procedure done in the hospital. Noted to have some bleeding and hematoma after TR band removal which stopped with manual pressure. She is accompanied by her daughter who prompted the visit to the ED due to increasing swelling and new blisters that developed last night. The patient otherwise denies fevers, cough, nausea, vomiting, diarrhea.
Vitals:
BP 128/70 | HR 76 | RR 16 | T 36.7 C | SpO2 97% RA
Pertinent Physical Exam Findings:
EXTREMITIES: ,(+) 2+ radial pulses. (+) fluctuant mass with an overlying blister. (+) ecchymosis noted to the hand and upper ulnar aspect of the forearm with erythematous lesions without warmth noted.
POCUS time!
Let’s take a look at what might be present within the soft tissues. You grab your handy dandy ultrasound and…
This was our initial view of the right wrist on ultrasound.
The radial artery (circled) is visualized at a depth of ~1.3 cm just to the right of the midline of the image.
Sliding the probe superiorly and inferiorly revealed a well circumscribed, complex, hypoechoic structure present just lateral (to the left) of the radial artery.
Review: When performing POCUS for most MSK or vascular applications, a high frequency linear transducer is typically used for better visualization of superficial structures. T
he probe marker should be oriented to the patient’s right or cephalad.
Don’t forget to decrease the depth of the image to improve your resolution and obtain both short and long-axis views of your target structures.
Using color doppler, there was evidence of blood flow within the hypoechoic structure, with a clear connection to the radial artery.
(Short-axis view of the right wrist with color doppler)
(Long-axis views of the right wrist with color doppler, bottom image shows the classic “yin-yang” sign which will be discussed below)
Based on the findings above, what diagnoses are on our differential?
As you can see, many pathologies can share similar features on basic ultrasound. You should always apply color doppler to hypoechoic/anechoic structure to differentiate them from other fluid-filled structures such as blood vessels, the gallbladder, medullary pyramids, urinary bladder, etc.
The eventual diagnosis for this patient was a pseudoaneurysm of the right radial artery.
Radial artery pseudoaneurysms (RAPs) are rare, with an overall incidence of approximately 0.009% after transradial catheterization.
The most common causes are iatrogenic injuries from arterial cannulation or catheterization, accounting for about 80–90% of cases.
Traumatic injuries (blunt or penetrating) contribute roughly 5–10%, while infections, inflammatory conditions, and connective tissue disorders each account for less than 5% of RAPs.
Iatrogenic causes remain the predominant etiology, with trauma and other causes being much less frequent.
The underlying pathophysiology of pseudoaneurysms is due to a breach in the arterial wall (intima and media).
The blood escapes the lumen and is contained only by adventitia or perivascular tissue, forming a sac that communicates with the artery via a narrow neck.
What exactly are we looking for on ultrasound?
Ultrasound is the first-line imaging modality for radial artery pseudoaneurysms, with high diagnostic accuracy.
The best available evidence reports a sensitivity of 94% and specificity of 97% for pseudoaneurysms on ultrasound.
Below are some of the most notable sonographic features of pseudoaneurysms:
Hypoechoic sac with a narrow neck extending from the radial artery
“Yin-Yang” sign (turbulent bidirectional blood flow)
“To-and-fro” waveform of blood at the neck seen with spectral doppler
Here is a classic image of the characteristic “yin-yang” sign:
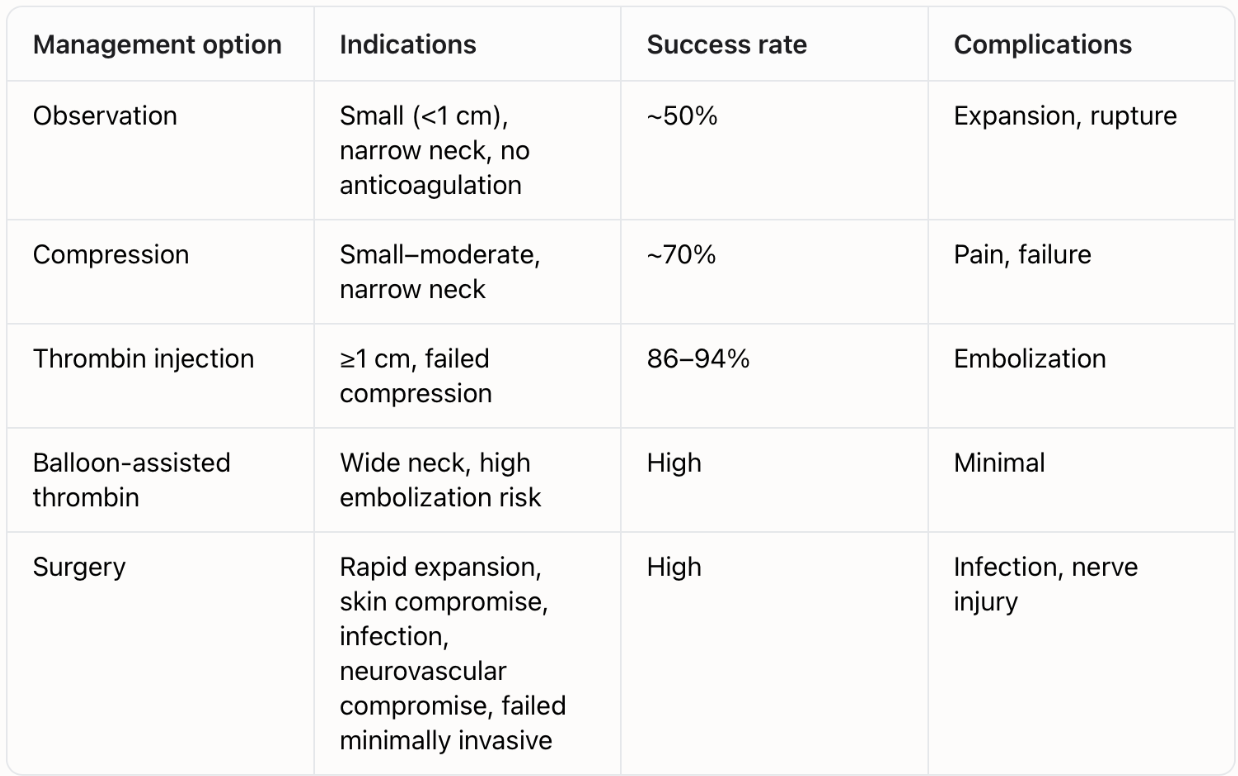
Management:
Vascular surgery consult (especially if within 60 days of surgery)
Observation may be appropriate for small (<1 cm), narrow-neck pseudoaneurysms without anticoagulation or infection, however spontaneous thrombosis may occur.
Repeat the ultrasound at 24–48 hours and 1–2 weeks to monitor for recurrence, thrombosis, or embolization.
Anticoagulation: Resume cautiously after hemostasis.
Some patients may require further interventions, such as:
Thrombin injection: First-line for pseudoaneurysms ≥1 cm or failed compression.
Balloon-assisted thrombin: Used for wide-neck lesions to reduce the risk of embolization.
If conservative or minimally invasive therapy fails, the definitive treatment is surgical exploration and repair with ligation or grafting performed by vascular surgery.
Key point: Start with conservative or minimally invasive options in stable patients; escalate to surgery if there is rapid expansion, skin compromise, infection, neurovascular compromise, or failure of less invasive therapy.
Back to our case:
Vascular surgery was consulted and a pressure dressing was applied to the forearm.
The patient was admitted to the hospital and underwent right radial artery exploration and primary repair of a pseudoaneurysm five days after presenting to the ED.
Right hand perfusion was noted to be intact with appropriate sensory, strength, and motor function.
Cardiology was also consulted and recommended to continue ASA, plavix, and hold eliquis. Heparin was resumed.
She was ultimately stable for discharge home without further complications.
Key Takeaways of this case:
Always suspect radial artery pseudoaneurysm in patients with a history of recent radial access or trauma
Ultrasound enables early diagnosis and can guide management to prevent complications such as rupture or ischemia
Sonographic features of RPA include: “yin-yang” sign and “to-and-fro” blood flow on doppler studies
ED management involves observation, ultrasound guided-compression, and vascular surgery consult
Definitive treatment may require surgical repair.
Happy scanning!
References
Boumezrag M, Ummat B, Reiner J, Venbrux A, Sarin S. Pseudoaneurysm: a rare complication of distal transradial access in the anatomical snuffbox. CVIR Endovasc. 2019;2(1):21. Published 2019 Jun 29.
Hadad MJ, Puvanesarajah V, Deune EG. Complications of Transradial Catheterization and Cannulation. J Hand Surg Am. 2019;44(11):973-979.
Kim D, Arbra CA, Simon Ivey J, Burchett P, Gonzalez G, Herrera FA. Iatrogenic Radial Artery Injuries: Variable Injury Patterns, Treatment Times, and Outcomes. HAND. 2019;16(1):93-98.
Shreve L, Jarmakani M, Javan H, et al. Endovascular management of traumatic pseudoaneurysms. CVIR Endovasc. 2020;3(1):88. Published 2020 Nov 27.
Dryton G, Allen KB, Borkon AM, Aggarwal S, Davis JR. Do not bite the hand that feeds you. Ann Vasc Surg. 2015;29(2):362.e3-362.e362004.
Habiyaremye TD, Alloy AC, Gibbons RC. Finding the balance: the point-of-care ultrasound diagnosis of pseudoaneurysm. J Emerg Med. 2024;66(2):e61-e64.
Kumar A, Kumar A, Kumar A, et al. A rare case of radial artery pseudoaneurysm following percutaneous coronary intervention. Clin Case Rep. 2023;11(10):e8725.
Kumar A, Kumar A, Kumar A, et al. Radial artery pseudoaneurysm: a rare complication of arterial line placement or cardiac procedures. J Hand Surg Am. 2017;42(5):e337-e341.
Cauchi MP, Robb PM, Zemple RP, Ball TC. Radial artery pseudoaneurysm: a simplified treatment method. J Ultrasound Med. 2014;33(8):1505-1508.
Garvin RP, Ryer EJ, Yoon HR, et al. Ultrasound-guided percutaneous thrombin injection of iatrogenic upper extremity pseudoaneurysms. J Vasc Surg. 2014;59(6):1664-1669.
Gregory M, Guest M, Abdeen I, Steiner K. Balloon assisted, ultrasound guided percutaneous thrombin injection of a large radial artery pseudoaneurysm using a trans-venous approach via an ipsilateral arteriovenous fistula. CVIR Endovasc. 2021;4(1):16.