PENG BLOCK
Written by: Dr. Justin Song
Edited by: Dr. Joann Hsu
The Case
81F PMH asthma, HTN, HLD, chronic PE on Eliqius, Alzheimer’s (AOx1 at baseline) presenting to ED for left hip pain s/p fall 3 days ago at her nursing home. Pain is exacerbated by movement and she denies any new numbness or weakness.
Pertinent exam: EXTREMITIES: (+) left leg mildly shortened, no rotation, non-tender palpation of left hip, no overlying ecchymosis, swelling, or laceration, strong DP pulse, good capillary refill
Imaging: CT pelvis - acute left femoral neck fracture, masslike thickening centrally within the uterus, layering bladder stones
Pelvic and femur XR - acute left femoral neck fracture with impaction
Disposition
Ortho was consulted and after reviewing risks and benefits of surgery vs nonoperative management, patient’s daughter elected to proceed with non-operative management and pain control as needed for the left femoral neck fracture.
The patient will return to the nursing home and follow up with trauma orthopedics outpatient.
Our ultrasound team offered a PENG nerve block as non-opioid adjunct to pain management and the daughter agreed.
What is PENG?
PENG stands for Pericapsular nerve group (PENG) block.
This is a plane block where local anesthetic is injected into the fascial plane between the psoas muscle and iliopubic eminence (IPE). The target space is just underneath the hyperechoic psoas tendon where it abuts the IPE.
It is a good alternative to other regional blocks such as femoral nerve (FN) blocks and fascia iliaca compartment block (FICB) for IT and femoral neck fractures.
The PENG block has the advantage of lower incidence of motor weakness/blockade compared to other hip nerve blocks.
It is also a good option for elderly patients who may have atrophied muscle and less definable fascia as it theoretically reduces the risk of nerve damage or intramuscular injection since the ilium provides a tactile backstop for the operator. Some find the PENG technically easier than the fascia iliaca for this reason.
What is the PENG good for?
More on the specific anatomy in the next section, but the PENG is used for IT, femoral neck, pubic rami, acetabular fractures – aka proximal hip fractures.
PENG block does NOT cover below the IT level of the femur. The femoral nerve block and fascia iliaca are able to cover these more distal areas of the femur.
TL;DR:
You can use either PENG or fascia iliaca for IT and femoral neck fractures.
PENG may be a better option for older patients with poorly defined muscle/fascia anatomy.
Anatomy
The anatomy of the hip capsule can be divided into 2 parts: the anterior and posterior portions.
Nociceptors are highly concentrated in the anterior and superolateral capsule, while the posterior hip innervation is primarily composed of mechanoreceptors.
The target nerve for the PENG block are the sensory nerves located in the anterior hip and are the femoral nerve, obturator nerve, and accessory obturator nerves.
This spares the motor branches and proprioceptive fibers, reducing the likelihood of motor blockade compared to other nerve blocks.
Advantages include allowing patients to practice earlier range of motion or allow orthopedics to to perform motor function exams if the block is used for postoperative pain control.
Important anatomical landmarks in the procedure are the AIIS, femoral neurovascular bundle, iliacus muscle, psoas muscle and tendon, and pectineus muscle.
One limitation would be that the lateral femoral cutaneous nerve is not affected by this nerve block.
Protocol and Materials
The materials used in the PENG block are the same as any other hip block.
Item list can be found on the Kwalktalk page explaining the FICB procedure.
Important points to note from the list include the use of Ropivacaine without epinephrine as the choice of analgesic because it has reduced cardiotoxicity and longer duration of action compared to it’s long-acting counterpart bupivacaine and it’s shorter acting alternative, lidocaine.
Also, patients will need to be placed on telemetry and require lipid emulsion therapy at bedside in case of systemic anesthetic toxicity.
Preparing for the PENG block is easy, but the biggest barrier to completing the procedure may be finding a space to do the procedure and nursing staff to monitor the patient afterwards.
Technique
Patient is supine and the operator stands on the ipsilateral side as the fracture.
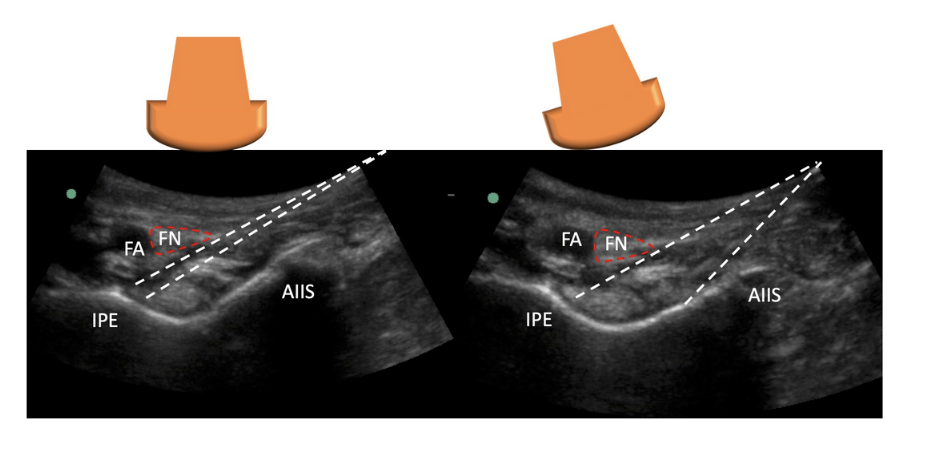
Using a curvilinear probe, start inferior to the inguinal ligament to visualize the femoral head.
The probe can be moved cranially until the AIIS and IPE is visualized.
Once the “trench” or the “divot” is identified, then you need to visualize the important landmarks: femoral artery, nerve, vein, iliacus muscle, and psoas tendon.
A 20+ gauge long spinal need will be used in a lateral-to-medial approach until the needle comes in contact with the ilium. This procedure is done with in line technique.
Target is the subfascial plane underneath the psoas tendon/above the ilium.
Area can be hydrodissected with normal saline to help correctly identify the correct location before pushing the anesthetic.
Deposit 20-40 mL of your long acting anesthetic into this space.
Your volume will depend on your anesthetic concentration.
Since this is a plane block, we aim for higher volume of anesthetic and thus a lower concentration to avoid toxicity.
We typically use 30-40 mL of 0.25% ropivacaine without epi for the PENG block.
Always calculate the max dose of anesthetic for your patient based on weight, choice of anesthetic, and comorbidities. The app “safe local” is a great resource for this.
It is important to visualize the needle tip during the procedure.
Remember the probe is already in the ideal position with all the landmarks identified, so the needle will have to be corrected with micromovements to stay in the window of the probe.
In a successful block, you will be able to lift the psoas tendon off the ilium and see the anesthetic track laterally and medially.
A good way to optimize the procedure to avoid injuring the femoral neurovascular bundle would be rocking the US probe to create a wider window for you to start at a steeper needle angle.
Clips from our PENG block for this patient:
Identification of the AIIS, IPE, and femoral neurovascular bundle in the left hip
Color flow to confirm femoral neurovascular bundle.
Inserting needle towards the psoas tendon.
Injection of local anesthetic into the facial plane beneath the psoas tendon.
Happy scanning!
References
Ben Aziz, M., & Mukhdomi, J. (2023, February 28). Pericapsular Nerve Group Block. StatPearls. Retrieved September 4, 2024, from https://www.ncbi.nlm.nih.gov/books/NBK567757/
Berlioz, B. E., & Bojaxhi, E. (2023, January 29). PENG Regional Block. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK565870/
How I do it: PEricapsular Nerve Group (PENG) block. (2023, August 1). ASRA Pain Medicine. https://www.asra.com/news-publications/asra-newsletter/newsletter-item/asra-news/2023/08/01/how-i-do-it-pericapsular-nerve-group-(peng)-block
Nutovits, A., & Chang, K. (2019, September 30). Fascia iliaca block (A. Elagandhala & V. Huang, Eds.). Kwak Talk. Retrieved September 4, 2024, from https://kwaktalk.org/block-talk/2022/12/27/fascia-iliaca-block
Pericapsular Nerve Group (PENG) Block - An Evidence Based Discussion : Virtual Library. (2022, August 16). WFSA Resource Library. https://resources.wfsahq.org/atotw/pericapsular-nerve-group-peng-block-an-evidence-based-discussion/
Pericapsular Nerve Group (PENG) Block for patients with hip or pelvis fractures in the ED. (n.d.). EM Ultrasound Section. https://www.acep.org/emultrasound/newsroom/apr2021/pericapsular-nerve-group-peng-block-for-patients-with-hip-or-pelvis-fractures-in-the-ed