I Googled Eye Puns But Couldn’t Find Any That Weren’t Cornea
Written by: Dr. Rebecca Zhang
Edited by: Dr. Joann Hsu
The case:
26 year old male with no PMHx presents to ED for sudden onset left-sided vision loss x 2 days after waking up. Patient states that his head has been hurting but denies other symptoms such as eye pain. He woke up that morning feeling like his left eye became very blurry. Reports his right eye has been fine. No fever, chills, headache, dizziness, nausea, or vomiting.
The exam:
Patient is awake, alert, and in no acute distress.
SKIN: Warm, dry; (-) cyanosis; (-) rash.
HEAD: (-) scalp swelling, (-) tenderness.
EYES: (-) conjunctival pallor, (-) scleral icterus, (+) visual acuity is 20/20 OD and unable to assess OS as patient cannot visualize Snellen's, (+) right-ward deviation of the left eye with concentration, (+) left eye minimally more dilated than the right but both reactive to light, (+) IOP OD 23.6 and OS 22.6,
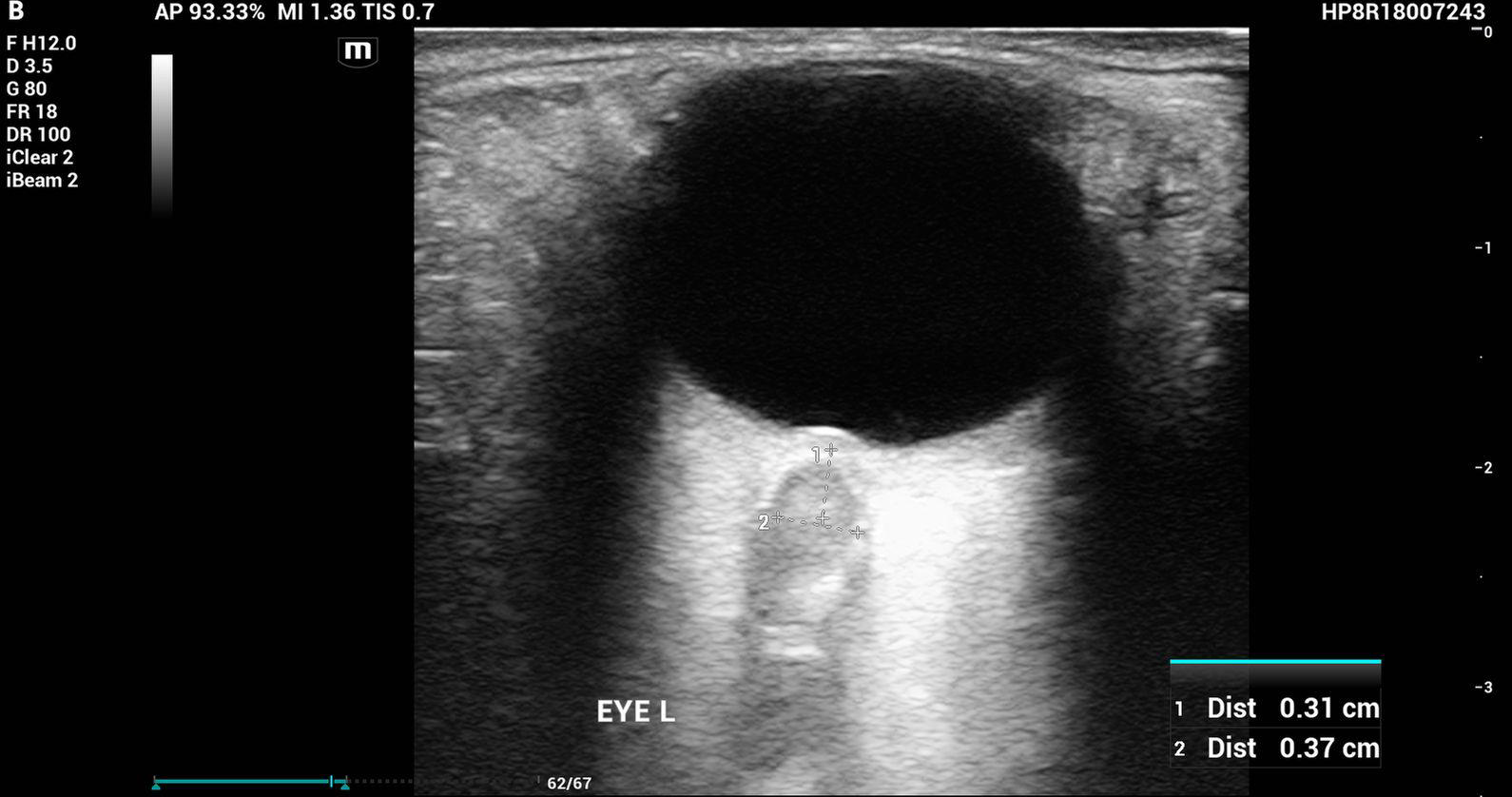
The bedside ultrasound:
Papilledema
Definition: Optic disc swelling due to increased ICP
Common Causes:
Malignant Hypertension
Idiopathic Intracranial HTN
Intracranial Mass
Hydrocephalus
Clinical Features
Headache worse in the morning
Nausea, vomiting
Back to the case:
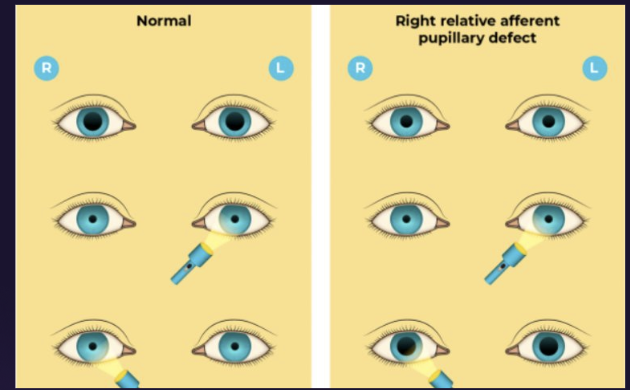
Ophthalmology was consulted and note a prominent afferent pupillary defect of the left eye on their exam
Combined with grade 4 optic disc edema, this is concerning for…
Optic Neuritis
Background/etiology
Inflammatory or demyelinating disease, associated with MS in young, female, caucasian patients
Idiopathic
Multiple sclerosis
Viral infections
Clinical features/Exam
Acute monocular vision loss occurring over days but usually within hours with retro-orbital headache and pain
Afferent Pupillary Defect
Normal IOP with papilledema on ultrasound
Disposition
Admit
Inpatient neurology workup and management
IV Solumedrol 1g QD x 3 days
Timeline of the case
Day 1: Presented to ED
Day 2: Quantiferon gold returns positive for latent TB, MRI orbits confirmed optic neuritis, CTA head neck, MRI brain normal, no stroke
Day 5: Discharged, visual acuity back to baseline!
Happy scanning!
Resources:
Voss E et al. Clinical approach to optic neuritis: pitfalls, red flags and differential diagnosis. Ther Adv Neurol Disord. 2011 Mar; 4(2): 123–134.
Shevlin C. Optic Nerve Sheath Ultrasound for the Bedside Diagnosis of Intracranial Hypertension: Pitfalls and Potential. http://www.criticalcarehorizons.com/optic-nerve-sheath-diameter-icp/