Retinal Detachment
Written by: Dr. Kristen Kobayashi
Edited by: Dr. Joann Hsu
The case:
A 66 year old female with no PMH presents to the ED with blurry vision in the right eye x 4 days. She denies pain or complete loss of vision. She denies headache, fever, numbness, tingling, weakness.
Her physical exam is significant for PERRL, EOMI, R IOP: 14, L IOP: 14, Visual acuity: HM OD, 20/40 OS, and an otherwise normal neurological exam.
Differentials to consider for painless vision loss include:
Amaurosis fugax
CVA
CRAO, CRVO
Retinal detachment
Vitreous detachment, vitreous hemorrhage
Complex migraine.
Your bedside ocular ultrasound images show a “mac off” retinal detachment with likely associated vitreous detachment.
“Mac on” retinal detachment is an emergent diagnosis that cannot be missed!!
Bedside ultrasound is a useful tool to evaluate for this diagnosis.
A recent meta-analysis in February 2020, “Ocular Point-of-Care Ultrasonography to Diagnose Posterior Chamber Abnormalities”, studied the sensitivity and specificity of Ocular POCUS by ED physicians evaluating a variety of abnormalities in the vitreous chamber.
They found that the sensitivity and specificity of ED physicians diagnosing retinal detachment was 94% and 94%, respectively.
This means ocular POCUS can be a great screening tool in low-risk patients to rule out retinal detachment, or a good diagnostic tool to rule in high-risk patients.
A linear probe should be utilized to evaluate the globes, given its high frequency and resolution for superficial structures.
You may use a large tegaderm over the eye and place gel over it, given the risk of conjunctival irritation and pain when ultrasound gel comes into contact with the eye.
It is important to anchor your hand while scanning to avoid placing too much pressure on the eye which can be uncomfortable.
Examples of a normal ocular ultrasound:
The anterior chamber, iris, lens, and optic nerve can be clearly visualized.
The vitreous chamber is anechoic without internal echos.
In a retinal detachment, a thick, hyperechoic membrane that is tethered to the optic nerve can be visualized in the vitreous chamber as shown below:
The patient will possible complain of a “curtain-like” vision loss, floaters, or flashes.
It is important to scan through the entire globe in both transverse and sagittal planes because when cut at certain angles, a retinal detachment may be confused for a vitreous detachment.
At this point, an emergent ophthalmology consult should be placed.
To provide your consult extra information, you can evaluate whether the retina is still attached to the macula or not (“mac on” vs “mac off”).
The macula is located just temporally (laterally) to the optic nerve.
It can be found at the intersection between a line made from the anterior chamber and lens to the posterior globe.
An example of “mac on” retinal detachment:
Notice the tethering occurs just temporal of the optic nerve, which could mean that it is still attached at the macula.
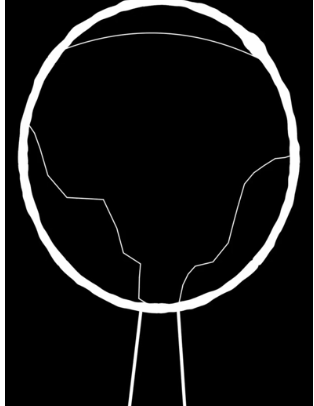
An example of “mac off” retinal detachment:
Notice the tethering occurs at the optic nerve
A big caveat to this mac-on vs. mac-off discussion: your bedside ultrasound is not considered diagnostic! It is helpful for collecting information but at the end of the day, you must consult ophthalmology when there is any clinical suspicion for retinal detachment.
Vitreous detachment on POCUS can look similar however the membrane appears thinner and does not attach posteriorly to the retina.
Patients will complain of cloudy vision, floaters, and flashes.
Vitreous detachments can increase the patients risk for retinal detachment so an ophthalmology consult should be placed urgently.
An indirect ophthalmoscope exam by the ophthalmologist is the gold standard and best way to diagnosis either of these disease entities. I
In a patient with acutely worsened visual acuity, an ophthalmology consult should be placed for further evaluation given the poor sensitivity of ocular POCUS in detecting vitreous detachment.
Bedside ocular ultrasound has good sensitivity and specificity for detecting retinal detachments and is a technically simple test to increase a clinicians suspicion for ocular pathology.
Happy scanning!
References:
https://www.pocus101.com/ocular-ultrasound-made-easy-step-by-step-guide/
https://www.thepocusatlas.com/ocular-atlas
https://www.coreultrasound.com/vd-rd/
https://www.acep.org/sonoguide/advanced/ocular-emergencies
Propst SL, Kirschner JM, Strachan CC, et al. Ocular Point-of-Care Ultrasonography to Diagnose Posterior Chamber Abnormalities: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020;3(2):e1921460. doi:10.1001/jamanetworkopen.2019.21460