Upper Ext DVTs
Written by: Vidhi Rao, MD. Edited by: Jeff Greco, MD
Multiple protocols for ultrasonography of lower extremity deep vein thrombosis have been well-studied, but there is considerably less literature describing an ultrasound protocol to evaluate and diagnose DVTs in the upper extremities. Upper extremity DVTs account for as much as 8-10%1,2,3 of all DVTs but is associated with higher morbidity and mortality4. UEDVTs are almost always secondary to foreign body such as indwelling PICC line, conditions associated with hypercoagulability (i.e. malignancy, inflammatory states), ovarian hyperstimulation, or chronic diseases (heart disease, renal failure)1,4. CT or MR venography is considered the gold standard for diagnosis but POCUS offers a quick, inexpensive, and noninvasive alternative.
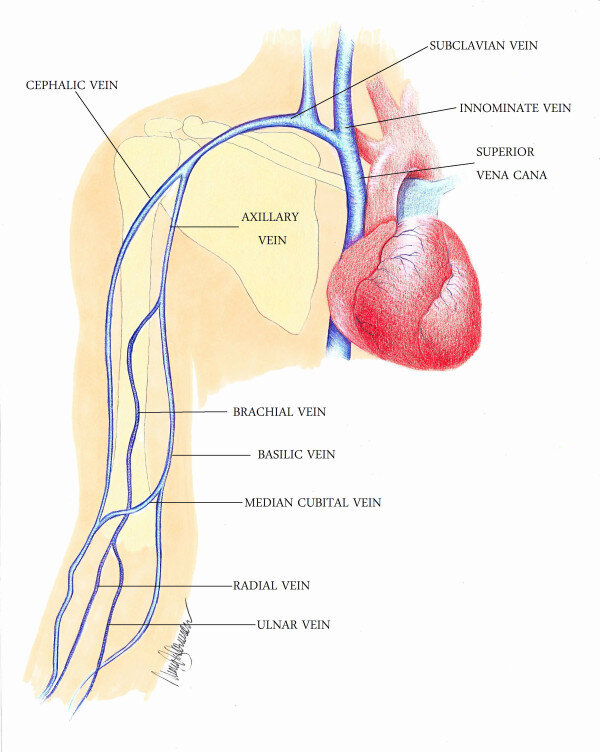
Anatomy
As a general rule of thumb, UE deep veins have an associated artery and accordingly include: brachiocephalic vein, internal jugular vein, cephalic vein, axillary vein, brachial vein (sometimes paired), and paired radial and ulnar veins. These latter distal veins are less frequently involved and are not routinely included in the evaluation.
Figure 1. Anatomy of deep veins of the upper extremity. Source: Rosen et al, 2012.
Patient positioning
Patient should be positioned supine with arm abducted 45-90’ and externally rotated. Head of bed may be elevated to 30’ and Trendelenburg position may be used to further optimize distension and visibility of upper extremity veins.
Figure 2. Patient positioning during sonographic evaluation of UE DVT. Source: Avila, 2020.
Technique
As with lower extremity DVT sonography, the “unaffected” upper extremity should be evaluated first to assess for differences. A distal-to-proximal approach is described here, but the sonographer may also elect to evaluate the vasculature from proximal to distal.
Using a high-frequency linear probe, evaluate the deep veins of the upper extremity starting just proximal to the antecubital fossa. Pulsed-wave or color flow may be applied to differentiate brachial vein from artery. Follow this distal portion of the brachial vein proximally along the axillary vein, sequentially applying and releasing gentle compression to fully collapse the vessel at 1-2cm intervals until arriving at the subclavian vein, which will be adjacent to subclavian vein and superficial to pleura.
Figure 3. Normal axillary vein and artery. Source: The POCUS Atlas, by Dr. Gordon Johnson.
Figure 4. Thrombosis of axillary vein in short axis. Source: Rosen et al, 2012.
Figure 5. Thrombosis of axillary vein in long axis. Source: Rosen et al, 2012.
The subclavian vein is usually best visualized from the infraclavicular approach but the central arching portion may be better visualized from the supraclavicular approach. As the vasculature underlying the clavicle is not compressible, any venous occlusion in the subclavian or brachiocephalic veins can be assessed with color flow and pulsed-wave Doppler when the vessel is visualized in longitude. Flow normally varies with respiration due to changes in intrathoracic pressure; absent or decreased variation compared the unaffected side suggests obstruction proximal to probe. Similarly, color Doppler can demonstrate diminished venous filling.
Figure 6. Abnormal (left) and normal (right) Doppler pulse-wave form. Source: Avila, 2020.
Finally, visualize the internal jugular vein and evaluate with direct compression or Doppler. Optionally, the sonographer may wish to evaluate the distal, less-frequently-involved deep veins (radial and ulnar) or the larger superficial veins (brachial and cephalic veins) in certain clinical scenarios.
Figure 7. Compression of internal jugular vein, normal finding. Source: Avila, 2020.
Figure 8. Thrombus of internal jugular vein. Source: The POCUS Atlas, by Dr. Renato Tambelli.
Summary
The principles and techniques in performing assessing upper extremity DVT is similar to those of lower extremity DVT sonography. Sonographic findings suggesting DVT include:
Directly visualizing echogenic clot
Inability to compress vein completely
Asymmetrical venous distension relative to adjacent artery
Reduction in or absence of flow variation with either respiration or distal augmentation on pulse wave Doppler
Filling defect (decreased or absent flow) on color flow Doppler
It is important to note that absence of these findings may not be sufficient to rule out DVT. Older studies have shown US sensitivity and specificity to be 82% each[4], although these have more recently been determined to be as high as 97% and 96% respectively[3]. Meanwhile, the sensitivities of CT and MR venography have been reported as 95.9%[4] and 100%[3], respectively. In the event that POCUS is negative but clinical suspicion remains high, consider performing a contrast study with CT or MR venography to exclude UEDVT.
Sources:
1. Patterson J, Goodsell K, Herbst M, Vermeulen M. Cases That Count: Left Arm Swelling. Acep.org. https://www.acep.org/how-we-serve/sections/emergency-ultrasound/news/september-2018/cases-that-count-left-arm-swelling/. Accessed January 29, 2021.
2. Extremity Swelling - Upper Extremity DVT. https://www.med-ed.virginia.edu/courses/rad/edus/es2.html. Accessed January 29, 2021.
3. Grigorian A, Nahmias J. Upper Extremity Deep Venous Thrombosis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482420/. Published 2020. Accessed January 29, 2021.
4. Mullens C, Minardi J, Denne N, Dorinzi N, Setzer E. Subclavian DVT: Diagnosis In Seconds With POCUS. https://digital.graphcompubs.com/publication/?m=30875&i=437924&view=articleBrowser&article_id=2882232&ver=html5. Accessed January 29, 2021.
5. Rosen T, Chang B, Kaufman M, Soderman M, Riley D. Emergency department diagnosis of upper extremity deep venous thrombosis using bedside ultrasonography. Crit Ultrasound J. 2012;4(1). doi:10.1186/2036-7902-4-4
6. Avila J. 5 Minute Sono – Upper Extremity DVT.; 2020. https://www.coreultrasound.com/5ms_uedvt/. Accessed January 29, 2021.
7. Johnson G. Axillary Vein (Normal Compressible). The POCUS Atlas. https://www.thepocusatlas.com/dvt/zrwjzsr6wmf7w9ha87xw6pecnw8384. Published 2021. Accessed January 29, 2021.
8. Tambelli R. Internal Jugular Thrombus. The POCUS Atlas. https://www.thepocusatlas.com/dvt/internal-jugular-thrombus. Accessed January 29, 2021.