Fascia Iliaca Block
Written by Ari Nutovits MD and Kenneth Chang DO. Edited by Dr. Akshay Elagandhala and Dr. Victor Huang
Introduction
The ultrasound-guided fascia iliaca compartment block (USGFICB) is an alternative approach to establish a peripheral lower extremity nerve block compared to the femoral nerve and lumbar plexus blocks that have been done previously.[1]
Prior to using ultrasound, the technique was primarily done by anesthesia and was a landmarked based approach, similar to doing a lumbar puncture, you would feel a “double-pop” technique as the needle would pass from the fascia lata through the fascia iliaca.
This technique can block “3 in 1” nerves- the obturator, femoral, and lateral femoral cutaneous nerve, so it is very effective for any injuries to the hip, anterior thigh, femur and patella.
This technique would be preferable to our elderly population who are typically on more medications, and instead of giving narcotics with can cause respiratory depression this is an alternative longer lasting approach.
The ultrasound guided femoral nerve block (USGFNB) in my opinion should be a first line approach used in the Emergency Department (ED), as the effects are long lasting for pain control and it’s a well-researched approach for controlling pain in hip fractures or femur fractures.
The analgesic effect of fascia iliaca compartment blocks as a whole was found to be superior to that of opioids, which resulted in lower preoperative analgesia consumption and a longer time for first request, and reduced time to perform spinal anaesthesia.[2]
Studies have shown that the reduction in opioid usage in this elderly patient population, with an average age of seventy five years, has produced alert and mobile patients often as early as post-operative day one with significant decrease in overall pain score compared to that of opiods.[3]
The Basic Anatomy
As shown in this figure, the target site of injection is 1/3 the distance from the ASIS to the medial end of inguinal ligament.
Femoral neck receives most of its sensory innervation from the articular branches of the femoral nerve, with minor contributions from obturator and gluteal nerves.
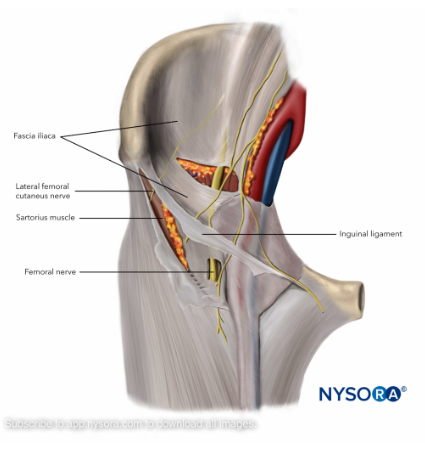
The femoral nerve is the most easily identified, located just lateral to the femoral artery and vein, on top of the iliacus muscle. It is separated from the femoral artery by the fascia iliaca.
The femoral nerve and the obturator nerve both transverse a compartment that spans the lower abdomen and anterior thigh and are confined anteriorly by the fascia iliaca.
Obturator nerve runs through the psoas muscle and wraps behind the common iliac vessels, innervating only a small portion of medial aspect of leg. It is only sometimes blocked with this technique.[4]
The lateral femoral cutaneous nerve is posterior to the lateral aspect of inguinal ligaments, innervating the lateral aspect of the thigh.[5]
The sciatic nerve innervates the posterior compartment of the thigh and is not blocked by anesthetic injection anteriorly, as described in this technique. 3
The fascia iliaca runs below the fascia lata and is the second fascial plane encountered when viewing the proximal lower extremity under ultrasound. It runs anterior to the iliacus muscle, psoas muscle, and pectineus muscle. The sartorius muscle, as well as the femoral vessels, are located between the fascia lata and the fascia iliaca. 2
There may also be 2 “pops” felt while gaining access to each of the fascial planes.
The fascia iliaca compartment block has the potential to create a sensory block of the femoral, obturator, genitofemoral, and lateral femoral cutaneous nerves.
The nerve blocks from this technique are achieved by injecting local anesthetic into the compartment lateral to the femoral nerve, which lies lateral and adjacent to the vascular bundle.
The 2 approaches of performing the USGFICB are from suprainguinal and infrainguinal.
Expected area of fascia iliac sensory block (Mainly lateral femorocutaneous and femoral nerve)
Our Protocol [6][7][8]:
ED Protocol:
1. ED Physicians should offer this procedure to all patients with proximal femur fractures after discussion with the Orthopedist on-call.
2. If the ED is unable to perform this procedure, the Anesthesiologist on-call should be contacted for this procedure.
Set Up:
❏ Informed Consent
❏ Time-out
❏ Location with appropriate space and monitoring where the procedure can be performed:
❏ Procedure Room
Monitoring:
❏ Cardiac monitor, continuous pulse oximetry, blood pressure
❏ 1:1 Nursing, as in procedural sedation
❏ RN trained to monitor for cardiovascular and neurologic sequelae of lidocaine toxicity who is available to monitor the patient continuously for 30 minutes.
❏ Pre- and post-procedure vital signs and neurovascular checks
Materials:
❏ Ultrasound machine with a high-frequency linear probe (6 - 14 MHz)
❏ Sterile probe cover and gel
❏ Sterile gloves, sterile field, chlorhexidine
❏ Second provider present for assistance
❏ Lidocaine 1% in a 10 mL syringe to anesthetize the entry site
❏ 20 - 40 mL syringe and IV tubing
❏ 3-way stop cock with attached 10 mL syringe of normal saline
❏ 20 - 22 gauge echogenic or spinal needle
❏ Local anesthetic: 20 - 40 mL of dilute anesthetic
❏ Ropivacaine 0.5% (Preferred local anesthetic due to its long-acting duration, greater safety profile, reduced cardiotoxicity). *Maximum dose of 3 mg/kg (without epinephrine)
❏ Bupivacaine 0.25% *Maximum dose of 1.75 mg/kg (without epinephrine)
❏ Code cart available: AED, airway supplies, ACLS and anti-seizure medications.
❏ Lipid emulsion therapy
❏ Intralipid: fat emulsion 20% injection, 500 mL bag (in Trauma Pyxis)
❏ See attached checklist: ASRA 2018 Checklist for the Treatment of Local Anesthetic Systemic Toxicity (LAST)
Complications of the Procedure:
Local Anesthetic Systemic Toxicity
a. A rare but life-threatening complication of large-volume local anesthetic injections.
b. Reduce the risk of LAST by using ultrasound needle guidance, and aspirate before injecting to prevent unintentional intravascular injection of local anesthetic.
c. Minor Symptoms: perioral numbness, paresthesia, tinnitus, muscle fasciculations
d. Neurologic: tonic-clonic seizures, global CNS depression, coma.
e. Cardiovascular: hypotension, bradycardia, conduction defects, ventricular dysrhythmias, respiratory and cardiac arrest.
2. Infection
3. Bleeding
4. Nerve or vascular injury
Infrainguinal Approach
Orient the linear transducer indicator cephalad after placing it perpendicular to the inguinal ligament.
Start at femoral artery and locate the hyperechoic femoral nerve, slide laterally to identify the sartorius (inferior) and the iliacus muscle (superficially).
The fascia lata and fascia iliaca should form a “bow tie” over the iliacus muscle.[9]
Place a skin wheal just caudal to transducer and insert the needle in an in-plane, long-axis approach.
Guide the needle below inguinal ligament, through fascia lata and fascia iliaca at the center of “bow tie.”
Aspirate, then start by injecting 2-3 mL of local anesthetic to confirm needle placement under US guidance.
Gently hydro-dissect the fascia iliac from the iliacus muscle (you’re in the correct spot!)
Gently inject 30-60 cc of local anesthetic in 5 mL increments, aspirating to avoid inadvertent vascular puncture.
In the infrainguinal approach, the fascia lata and fascia iliaca form a “bow tie” when overlapping between the sartorius caudad and internal oblique cephalad, with underlying iliacus muscle spanning over the ilium.7
Note the position of the probe: perpendicular to inguinal ligament and located 1/3 distance from ASIS to pubic symphysis, indicator cephalad and facing umbilicus.[10]
Suprainguinal Approach
Transducer is placed superior and parallel to inguinal ligament.
Slide probe more medially to visualize the femoral vein, femoral artery, and femoral nerve (similar to how you go about doing a femoral central line)
Move transducer laterally very slightly to visualize the sartorius muscle overlying the iliacus muscle.
Place skin wheal lateral to transducer, making location of the block where the needle will enter (or if you do not like to poke twice skip this step)
Needle is inserted in-plane, just lateral to transducer. Pathway should course through sartorius muscle or just superficial, sitting between the iliacus and fascia iliaca, lateral to neurovascular bundle (make sure to practice in-plane technique while doing US guided PIV before attempting this technique)
Once deep to fascia iliaca (you should feel a “pop”), aspirate, inject 2-3 mL of local anesthetic to confirm needle placement between the fascia and the iliopsoas muscle.
If you inject and see spread of local anesthetic above the fascia or within the muscle, stop and reposition the needle and attempt to inject 2-3 mL again.
Once position is confirmed, gently hydro-dissect with proper positioning 30-60 mL of local anesthetic in 5mL increments, gently aspirating to ensure vascular structures are not punctured.
A successful block should be visualized at all times and should show spread toward the femoral nerve medially and underneath the Sartorius muscle laterally.
This approach may be advantageous compared to the infrainguinal approach in blocking the LFCN, which leaves the fascia iliaca plane at level of inguinal ligament.
Using the infrainguinal approach included passing superiorly, which may lead to potential complications of bladder injury and arterial injury (deep circumflex inferior epigastric artery, external iliac artery, spermatic cord and hernia contents). Also, higher amounts of anesthetic are often needed if the infrainguinal approach were to be used to achieve same effect.[11]
The Suprainguinal View: Sartorius overlies the iliacus muscle on its lateral border, with the fascia iliaca separating the two muscles. The femoral nerve and vascular bundle lie medial to the iliacus muscle, and the lateral femoral cutaneous nerve lies between the muscle bodies.
Note: Approach of needle injection site using the suprainguinal approach is from lateral to medial, parallel to the inguinal ligament. Note the needle track ultimately ends between the fascia iliaca and the iliacus muscle, like in the infrainguinal approach.
Take Home Points:
USGFICB can be used for analgesia control in injuries of the hip, femur, patella and anterior thigh.
As winter approaches and the elderly population present with falls, think of using peripheral nerve blocks instead of narcotics for pain control.
This technique is less difficult than femoral nerve blocks, and potentially blocks the femoral, lateral femoral cutaneous and sometimes the obturator nerves.
Analgesia is injected in between the fascia iliaca and iliacus muscle in both the infrainguinal and suprainguinal approach.
In all these procedures, the systemic toxic dose of anesthetic must be considered with close neurological and cardiovascular monitoring during the procedure. The physician and nurse should always perform a time out, and the correct extremity should be marked and identified prior to the procedure taking place.
Discuss whether or not this procedure can be done with consulting services, in particular, orthopedics as it will affect their physical exam after it’s performed.
References:
1. Ultrasound-Guided Fascia Iliaca Block. NYSORA. https://www.nysora.com/regional-anesthesia-for-specific-surgical-procedures/lower-extremity-regional-anesthesia-for-specific-surgical-procedures/ultrasound-guided-fascia-iliaca-block/
2. Steenberg J, Møller AM. Systematic review of the effects of fascia iliaca compartment block on hip fracture patients before operation. Br J Anaesth. 2018 Jun;120(6):1368-1380. doi: 10.1016/j.bja.2017.12.042. Epub 2018 Apr 5. PMID: 29793602.
3. DULANEY-CRIPE, E., HADAWAY, S., BAUMAN, R., TRAME, C., SMITH, C., SILLAMAN, B., LAUGHLIN, R.. A Continuous Infusion Fascia Iliaca Compartment Block in Hip Fracture Patients: A Pilot Study. Journal of Clinical Medicine Research, North America, 4, jan. 2012. Available at: <https://www.jocmr.org/index.php/JOCMR/article/view/724/419>.
4. Ueshima, Hironobu MD, PhD*; Otake, Hiroshi MD, PhD. Supra-inguinal fascia iliaca block under ultrasound guidance for perioperative analgesia during bipolar hip arthroplasty in a patient with severe cardiovascular compromise. Medicine: October 2018 - Volume 97 - Issue 40 - p e12746
5. Pepe J, Madhani NB. Ultrasound-guided Fascia Iliaca Compartment Block. [Updated 2019 Apr 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK518973/
6. LaJeunesse M. Control hip fracture pain without opioids using ultrasound-guided fascia iliaca compartment block. ACEP website. https://www.acepnow.com/article/control-hip-fracture-pain-without-opioids-using-ultrasound-guided-fascia-iliaca-compartment-block/ . Published January 25, 2018.
7. Checklist for treatment of local anesthetic systemic toxicity (LAST). ASRA website. https://www.asra.com/content/documents/asra_last_checklist_2018.pdf .
8. Swaminathan A. Local anesthetic systemic toxicity (LAST). RebelEM website. https://rebelem.com/local-anesthetic-systemic-toxicity-last/ .
9. LaJeunesse, M. et al. https://www.acepnow.com/article/control-hip-fracture-pain-without-opioids-using-ultrasound-guided-fascia-iliaca-compartment-block/.
10. http://highlandultrasound.com/new-blog/2014/8/8/fascia-iliaca-block-for-hip-fractures.
11. Hebbard, P. Ivanusic, and Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia: 2011, 66, pages 300–305.