Hip Hop Pop: Open Fractures
Written By: Quinn Bushman, DO; Edited by: Timothy Khowong, MD, MSEd
Case Presentation
EMS report: A 72-year-old male with a history of HTN and HLD presents by EMS for ankle pain after sticking his leg in front of a moving car to stop it.
A tourniquet was applied on the scene due to “lots of bleeding” and “the foot being completely amputated” per EMS.
Upon arrival, the patient is in acute distress, screaming in pain, and he is alert and responsive. On physical exam, the patient has an exposed distal fibula and tibia that has punctured through the skin. A tourniquet has been applied proximal to the wound. No active hemorrhage. Pulses are not intact. Sensation is intact in the dorsal aspect of the foot, but decreased in the medial aspect of the foot. Pain medication was given, and labs were drawn.
Vital: T 38.1ºC, 144/76, P 112bpm, 97% on RA, RR 16
The tourniquet was brought down to evaluate the bleeding source. There was no active bleeding, neurological exam remained the same. Bedside XR was performed, showing displacement and fractures of the tibia and fibula.
A reduction was performed, then the wound was lightly irrigated and placed in a splint. The patient was given antibiotics, tetanus vaccination, IV fluids, and additional pain control. The patient was frequently reassessed for neurovascular changes before imaging
The patient was admitted to the orthopedics and trauma service for further management.
Open Fractures
Open fractures are defined as fractures in which the bone is exposed to the external environment through a disruption of the skin and subcutaneous tissues, resulting in a high risk of contamination and infection. The initial management of open fractures begins with prompt assessment and stabilization of the patient, including control of hemorrhage and evaluation for other life-threatening injuries.
Stabilization of injury requires a thorough evaluation of the neurovasculature of the distal aspect of the fracture. Prompt action must be taken to prevent long-term complications. A lack of prompt action results in increased risk of amputation and long-term complications, including chronic pain, necrosis of bone, weakness, and many other complications. Deficits of blood supply or neurological findings require prompt reduction. Active hemorrhage requires placement of a tourniquet for source control.
To place a tourniquet: Apply a tourniquet 2–3 inches proximal to the bleeding site (never over a joint), tighten until bleeding stops and distal pulses are absent, and secure the device in place. If bleeding persists, a second tourniquet may be applied immediately proximal to the first. Tourniquet use should be used for life-threatening extremity hemorrhage not controlled by direct pressure. Documentation and communication of application time is vital, as tourniquets should be removed prior to 6 hours of placement.
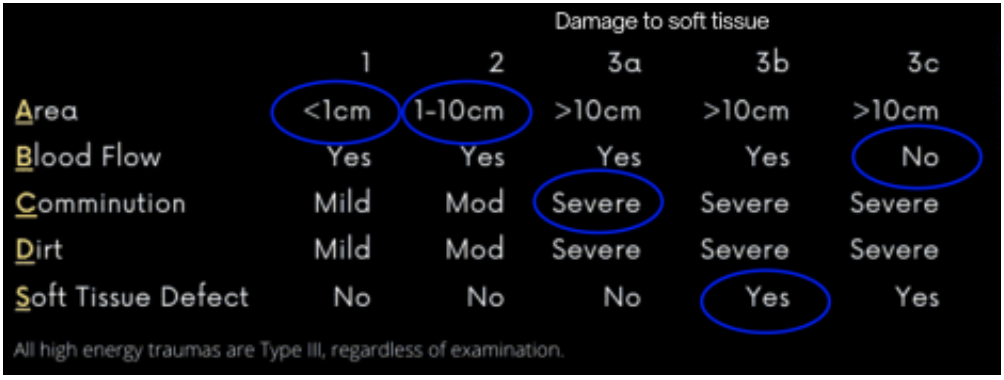
Once a patient is stabilized, further infection prevention is essential. Antibiotics within 1 hour, but no more than 3 hours, is the most effective method in preventing infection. Antibiotic choice is based on the Gustilo classification.
For most open fractures, the recommended first-line antibiotics are cefazolin or clindamycin (for those with beta-lactam allergy). For fractures including high-energy trauma and soft tissue injury (class III), the guideline recommends adding gram-negative coverage, with piperacillin-tazobactam. Other antibiotics should be considered if broader coverage is wanted.
● Soil or stool contamination → add penicillin (clostridium coverage) ● Fresh water contamination → add fluoroquinolone (aeromonas and pseudomonas coverage)
● Salt water contamination → add fluoroquinolone OR doxycycline + ceftazidime (vibrio, aeromonas, and pseudomonas coverage)
Tetanus status should be assessed on all patients and given promptly if indicated.
Patients are typically admitted to the trauma and orthopedics service for further management. Surgical irrigation and debridement should be performed within 24 hours of the injury.
Summary:
Open fractures are any fractures in which the bone is exposed to the external environment through a disruption of the skin and/or subcutaneous tissues.
Management:
• Early intravenous antibiotics: Administer as soon as possible, ideally within 1 hour of injury. For Gustilo-Anderson type I and II fractures, use a first-generation cephalosporin. For type III fractures, add gram-negative coverage. Consider adding other antibiotics for additional coverage.
• Tetanus prophylaxis: Assess immunization status and administer tetanus toxoid as indicated.
• Prompt surgical irrigation and debridement: Perform within 24 hours of injury, or sooner for gross contamination, vascular compromise, or compartment syndrome. Early debridement in the ED has not been associated with decreased infection risk
• Fracture stabilization: Achieve early stabilization, often with external fixation initially for severe injuries. Definitive fixation may be performed at the time of initial debridement if feasible.
• Ongoing assessment: Monitor for compartment syndrome and reassess for infection or nonviable tissue, with repeat debridement as needed.
Sources:
3) https://www.orthobullets.com/trauma/1004/open-fractures-management
4) https://journals.lww.com/jaaos/fulltext/2023/01010/aaos_clinical_practice_guideli ne_summary_.3.aspx