Total eclipse of the heart
Written by: Dr. Rozalina Suleymanova
Edited by: Dr. Joann Hsu
The Case:
49 year old male with past medical history of metastatic lung adenocarcinoma s/p radiotherapy and most recent chemotherapy session 2 weeks prior to presents to the ED with shortness of breath at rest and swelling of bilateral lower extremities and left arm for the last week.
Vitals:
BP 102/67
HR 97
RR 24
O2 93%
Physical exam:
Awake, alert, AO x3. In respiratory distress speaking in 2-3 word sentences
Lungs: decreased breath sounds to left lung field
MSK: pitting edema of B/L lower extremities and left upper arm to forearm
Beside ultrasound showed:
Parasternal long view
Parasternal long view with M mode- more on this later
Parasternal short view
A4 view
How do we know if a pericardial effusion has graduated to tamponade physiology?
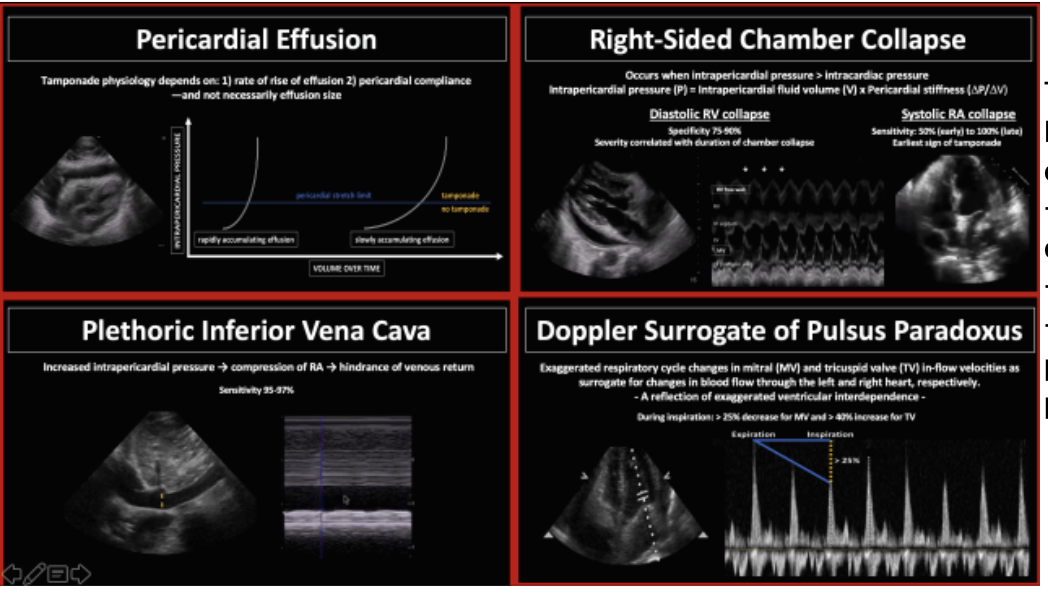
Tamponade = Pericardial effusion + RV diastolic collapse + Plethoric IVC + Sonographic pulsus paradoxus
** This is specifically talking about sonographic evidence of tamponade aka tamponade physiology. CLINICALLY, the patient would be hypotensive. Use your POCUS in conjunction with the clinical picture!
RV Diastolic Collapse
Studies generally show that RA systolic collapse is more sensitive than RV diastolic collapse in detecting tamponade, but RV diastolic collapse is more specific
RA systolic collapse has sensitivity 50-100%
RV diastolic collapse has sensitivity 48-60% and specificity 75-90%
The earliest sign of tamponade on ultrasound is RA systolic collapse however the RA is often more difficult to visualize on ultrasound, not to mention RA systolic collapse.
You can also use M mode (shown above) to objectively look for RV diastolic collapse in your PSL view.
Place the M mode line through the RV free wall and the tip of the anterior MV leaflet.
The point at which the MV begins to open (where it moves closer to the ventricular septum) is where diastole begins - this is highlighted in the boxes above.
You look at the RV free wall tracing closest to the top of the screen for evidence of RV wall collapse (downward movement, away from the probe) during diastole
Plethoric IVC
Obstructive pathology > compression of RA > reduced filling > reduced venous return > plethoric IVC
On ultrasound, measure at least 2 cm from the IVC/ RA junction.
≥2 cm + collapsibility less than 50% on inspiration = plethoric IVC
Plethoric IVC has a great sensitivity of 95-97% but specificity for tamponade is only 40% (recall that tamponade is not the only process with obstructive pathology causing plethoric IVC)
Sonographic Pulsus Paradoxus
Flow variation across the mitral valve using pulse wave doppler is the echo equivalent of the physiology that causes pulsus paradoxus
Place your pulse wave dopper gate over the mitral valve outflow to get this waveform seen above
Remember that PP = drop in systolic BP 10 mmhg with inspiration
A heart in tamponade shows increased ventricular interdependence, which means the dilation of one ventricle during inspiration affects the other.
Decreased filling = decreased LVEDV = decreased MV flow (sonographic PP)
Measure the largest and smallest E spike, which represents mitral inflow during inspiration and expiration.
If inflow variation is >25% across the mitral valve and >40% across the tricuspid valve, it is highly supportive for tamponade
TL;DR because we’re EM docs:
Ultrasound isn’t perfect and is VERY operator dependent, but it is still a useful adjunct to a good history and physical exam, so put a probe on it!
These are the sonographic signs to watch out for that can help support a diagnosis.
The disposition of our patient from the initial case:
CCU was consulted given the patient’s pericardial effusion and concern for tamponade. CCU admitted the patient under their service and the patient underwent pericardiocentesis at cath lab.
Happy scanning!