An ocular emergency?
Written by: Dr. Rita Kumar
Edited by: Dr. Joann Hsu
The Case
56 year old female presents to the ED with right eye pain after a physical altercation where she was punched in the right eye. Since then, she has had both eye pain and blurry vision in that eye.
Physical Exam
EOMI but with pain
mild periorbital swelling on the right eye
tenderness to palpation of the right periorbital area
right eye is fixed, dilated, and non-reactive to light
no teardrop pupil
Visual acuity: L 20/40 and unable to see Snellen chart with R eye or count fingers
Woods lamp exam: no signs of corneal abrasion
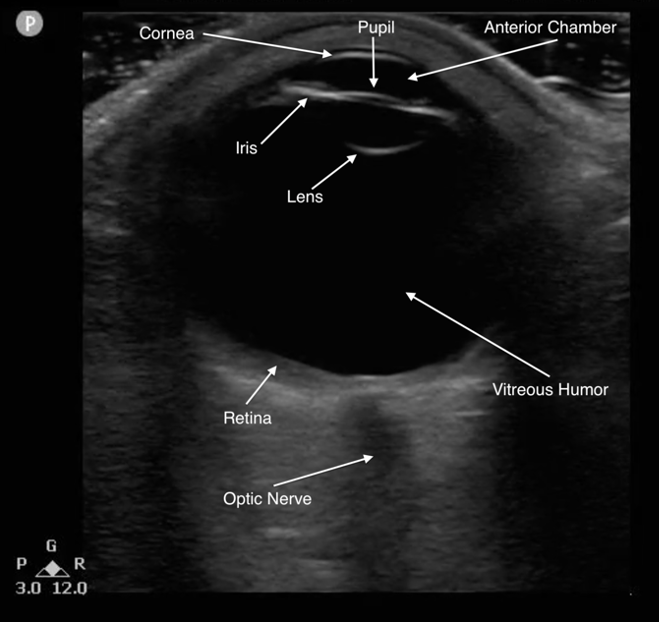
Ocular Ultrasound and Normal Anatomy
Before we perform a bedside US on our patient, let’s quickly review how to perform an ocular ultrasound and what normal eye anatomy looks like (1,3).
Technique:
Place patient head of bed at 45 degrees and apply copious amount of gel on top
The use of tegaderm over the eye to protect the eye is controversial.
Pro: “Protects” the eye, patient comfort
Con: May affect image quality
A 2022 study comparing tegaderm versus no tegaderm in ocular ultrasound showed no significant difference in patient comfort but did show reduced image quality
Marks A, Patel D, Chottiner M, Kayarian F, Peksa GD, Gottlieb M. Covered or uncovered: A randomized control trial of Tegaderm versus no Tegaderm for ocular ultrasound. Am J Emerg Med. 2022 Nov;61:87-89. doi: 10.1016/j.ajem.2022.08.044. Epub 2022 Aug 28. PMID: 36057214.
That being said – there is no official guideline so take it on a case by case basis!
Use the linear probe with minimal topical pressure – make sure to have it on ocular setting to minimize possible injury to the eye!
The ocular setting (or small parts) will have a lower thermal index
Gently scan the eye in transverse and sagittal planes, first static, then dynamic
Dynamic: Ask patient to look left/right or up/down to induce motion within the posterior chamber
Always compare with contralateral or unaffected eye to compare findings
**Note: if a globe rupture is suspected, an ocular US is contraindicated as pressure from the probe placed on the eye can potentially exacerbate injury. However, given this patient presentation and clinical exam, she had a very low suspicion for globe rupture based on external exam and thus it was safe to perform a bedside ocular US.
Normal eye anatomy:
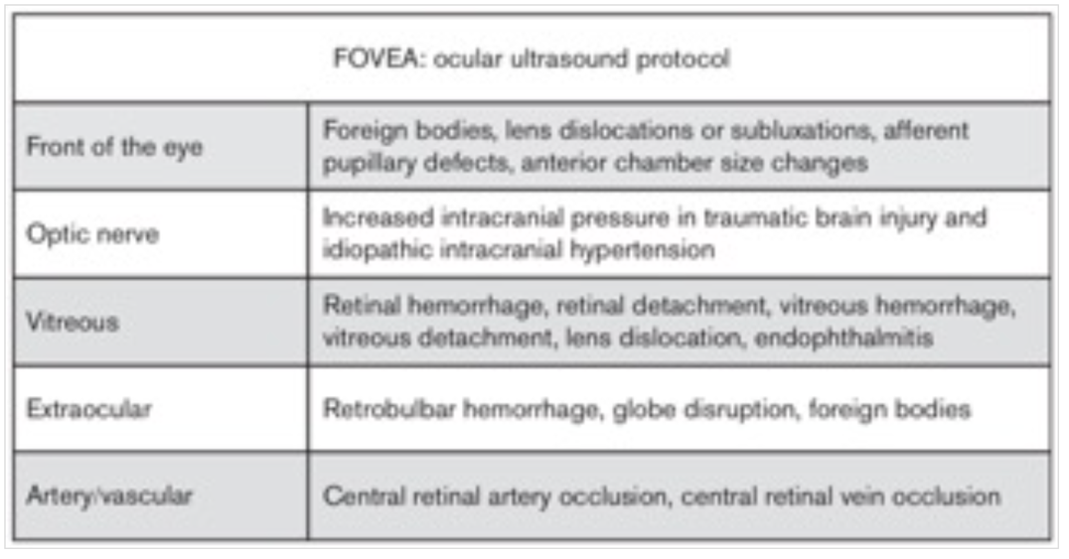
Here is a suggested scanning protocol provided by ACEP to identify eye pathology based on location and anatomy (3).
Back to the Case…
A bedside ocular ultrasound was performed on our patient and showed the following:
Unaffected left eye
Unaffected left eye
Right eye
Right eye
The clips of the right eye show the lens to be posteriorly displaced, floating within the vitreous humor—this is especially notable when you compare the placement of the lens with the left eye
Lens Dislocation
Anterior or posterior displacement of lens due to complete separation of lens zonule fibers
Usually due to blunt trauma to the eye
Can also occur in minor to no trauma in patients with: Marfan’s syndrome, homocystinuria, Ehlers-Danlos syndrome, tertiary syphilis, prior cataract surgeries
Classically presents as red, painful eye with associated diplopia or decreased visual acuity
Some patients may even complain seeing the outline of a lens in their eye (as our patient later confessed to)
If lens is anteriorly displaced, can obstruct aqueous flow, elevate IOP, and cause acute angle glaucoma4,5
Ultrasound findings (3)
Normal lens: hyperechoic, curved line located deep to the iris
Lens dislocation: generally, lens found floating in vitreous humor with eye movement or in posterior chamber. Can sometimes be in anterior chamber too
Management & Disposition
Optho consult (call emergently, especially if IOP is elevated)
They will decide to either repair surgically or observe, depending on displacement and associated injuries
This patient was assessed in the ED by ophthalmology and cleared for discharge to be follow-up outpatient in the eye clinic
Utility of Ocular Ultrasound Within the ED
Ocular complaints are common in the ED and recognizing which presentations may require emergent intervention can sometimes be challenging.
Slit lamp and fundoscopic exams are difficult to perform and may not be widely available in every ED.
However, bedside ocular ultrasounds are a fast and non-invasive exam to help differentiate between many ocular pathologies, including certain emergent ones.
Though ocular ultrasounds cannot be used to make a definitive ocular diagnosis, they can help narrow down differentials and allow one to act on emergencies faster.
This is especially important for a provider in terms disposition (i.e. emergent intervention requiring surgery/transfer OR safe discharge home).
This case is a great example of using POCUS to narrow down a diagnosis and facilitate management
Multiple studies have looked at the accuracy of ocular US within the ED, citing high specificity and sensitivity when compared to CT or ophthalmology
In this study , ED physicians were able to accurately identify ocular pathology using US in 60 out of 61 case when compared standard examination (i.e. CT or optho exam):
Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002 Aug;9(8):791-9. doi: 10.1111/j.1553-2712.2002.tb02166.x. PMID: 12153883.
With regards to lens dislocation, this study below found 84.6% sensitivity, 98.3% specificity, and 96.9% accuracy of ultrasonography in detection of traumatic lens dislocation:
Ojaghi Haghighi SH, Morteza Begi HR, Sorkhabi R, Tarzamani MK, Kamali Zonouz G, Mikaeilpour A, Rahmani F. Diagnostic Accuracy of Ultrasound in Detection of Traumatic Lens Dislocation. Emerg (Tehran). 2014 Summer;2(3):121-4. PMID: 26495362; PMCID: PMC4614573.
And here is a great schematic summarizing all the possible ocular pathologies you can find on US (9):
References
1. https://coreem.net/core/ocular-ultrasound/#overview
2. Habboushe J, Steinberg E. Eye Complaints. Basics of Emergency Medicine: A Chief Complaint-Based Guide. 2021;4:5
3. https://www.acep.org/sonoguide/advanced/ocular-emergencies
4. https://wikem.org/wiki/Lens_dislocation
5. https://www.aao.org/eye-health/anatomy/zonules
6. https://litfl.com/the-ocular-ultrasound-challenge/
7. Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002 Aug;9(8):791-9. doi: 10.1111/j.1553-2712.2002.tb02166.x. PMID: 12153883.
8. Ojaghi Haghighi SH, Morteza Begi HR, Sorkhabi R, Tarzamani MK, Kamali Zonouz G, Mikaeilpour A, Rahmani F. Diagnostic Accuracy of Ultrasound in Detection of Traumatic Lens Dislocation. Emerg (Tehran). 2014 Summer;2(3):121-4. PMID: 26495362; PMCID: PMC4614573.
9. https://www.pocus101.com/ocular-ultrasound-made-easy-step-by-step-guide/