Pseudoaneurysm Post-Cardiac Catheterization
Written by: Jessie Chen, DO; Edited by: Nate Zarider, MD
Case Presentation:
A 70-year-old male with PMHx of Atrial fibrillation on AC, CHF, DM, HLD presents for evaluation of pain, swelling and bruising to the right groin. He presents 6 days after completion of cardiac catheterization where the right femoral artery was used as the access site for his procedure. He reports a small growth in that region with associated bruising, but denies fevers, chills, warmth to the area. No pain down the lower extremity and no changes in strength or sensation of the affected leg. He is taking his newly prescribed DAPT and AC as usual. He told his cardiologist who suggested he go to the ER for evaluation of possible iatrogenic pseudoaneurysm.
Exam showed bruising to the right groin with a palpable thrill and a firm tender mass, similar to the image on the right. No overlying erythema, warmth. Neurological exam of the right leg was normal.
What is a Pseudoaneurysm?
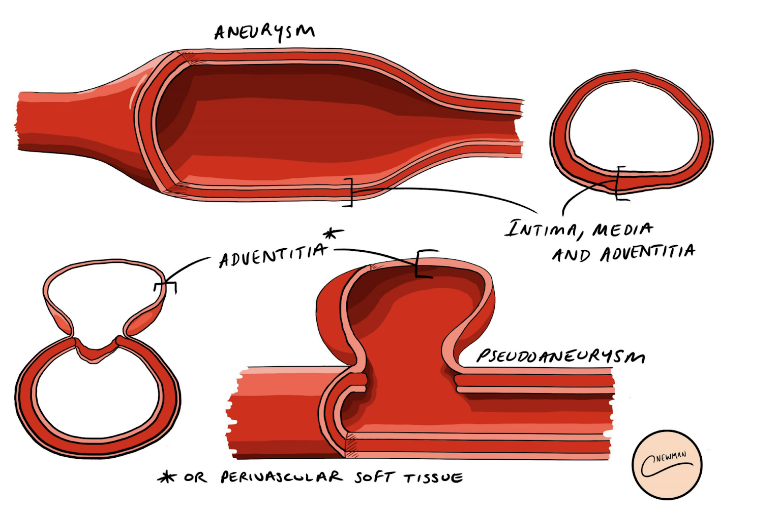
A pseudoaneurysm differs from a true aneurysm in that it does not involve all layers of the normal arterial wall. It most commonly only involves the adventitia. Sometimes the collection is walled off only by perivascular soft tissue.
The formation arises secondary to a disruption of all the layers of the arterial wall, in this case due to iatrogenic percutaneous vascular access and trauma. When the defect formed fails to be covered by a hemostatic plug, arterial bleeding occurs from the high pressure arterial system, leading to pseudoaneurysm formation.
Most Common Cause: Interventional Procedures
Most Common Site: Femoral Artery
Incidence: <1% of all interventional procedures
Diagnosis: Duplex Ultrasound
Duplex ultrasound has nearly 100% accuracy in diagnosing iatrogenic pseudoaneurysms and is the diagnostic imaging of choice.
Ying-Yang Sign: Seen on color doppler due to bidirectional flow between the femoral artery and the pseudoaneurysm lumen through the pseudoaneurysm neck. Aliasing is usually seen due to turbulent flow.
Below are the images from our patient’s bedside ultrasound:
Management:
There are two main ways to characterize Pseudoaneurysms:
Complicated vs Uncomplicated: Features that make a pseudoaneurysm complicated include:
Hemodynamic instablity
Neurologic deficit (motor or sensory)
Rapidly expanding hematoma
Extensive skin or subcutaneous damage
Signs concerning for superinfection
Size: Pseudoaneurysms greater than 3cm require intervention. Observation is recommended for all pseudoaneurysms less than 3cm. Intervention is not generally recommended for pseudoaneurysms smaller than one centimeter.
Observation involves repeat duplex ultrasound every 2 weeks for 6 weeks to evaluate for growth, acute symptoms, and assessment for complications (above)
One study showed most resolve by 2.5weeks. (1)
Treatment:
Ultrasound-guided Thrombin Injection (USTI) is the first-line treatment. Prior to USTI, US-guided compression to obliterate flow through the femoral pseudoaneurysm neck used to be the mainstay of therapy. But due to high failure rates, pain associated with the procedure, and the prolonged duration of the procedure (often requiring multiple attempts), USTI became favored. Data supports better overall success rates as well [cite the trial below].
Randomized trial of 32 patients: Thrombin injection vs Compression → At 24 hours, thrombosis higher in Thrombin Injection group (100% vs 13%). (3)
Case Resolution:
Patient was admitted to vascular surgery. Interventional radiology was consulted for ultrasound guided thrombin injection the following day. Patient had complete resolution of the pseudoaneurysm after thrombin injection and was discharged the following day.
References:
1.Toursarkissian B, Allen BT, Petrinec D, et al. Spontaneous closure of selected iatrogenic pseudoaneurysms and arteriovenous fistulae. J Vasc Surg. 1997;25(5):803-808; discussion 808-809. doi:10.1016/s0741-5214(97)70209-x
2. Stone P, Armstrong P. Femoral artery pseudoaneurysm following percutaneous intervention. In: Post TW, ed. UpToDate. Uptodate; 2022. Accessed November 20th, 2022. https://www.uptodate.com/contents/femoral-artery-pseudoaneurysm-following-percutaneous-intervention
3. Lönn L, Olmarker A, Geterud K, Risberg B. Prospective randomized study comparing ultrasound-guided thrombin injection to compression in the treatment of femoral pseudoaneurysms. J Endovasc Ther. 2004;11(5):570-576. doi:10.1583/03-1181.1