Gee, I Think This Patient Needs More Resuscitation
Written by: Alex Chu MD. Edited by Jeff Greco MD
The Case
62 yo M w/ hx cirrhosis w/ ascites, chronic EtOH presents with 2 d bloody emesis. He had a total of 5 episodes thus far and estimates he has seen about half a cup of blood total. Associated symptoms include diffuse abdominal pain, lightheadedness. Denies syncope, melena, hematochezia. No prior episodes. Last PO intake was this morning at 0900, 2-3 saltines. Last drink was yesterday, no prior hx of withdrawal requiring admission, DT, or seizures.
Vitals
T 37.6 C
BP 135/86
HR 94
RR 17 w/ O2 sat 97% on room air
Physical examination
Abdomen: Distended with fluid wave. Mild diffuse tenderness to palpation. No rebound or guarding. Caput medusae is observed. Bowel sounds present in all four quadrants.
Notable Labs
CBC - WBC 13, Hgb 9
BMP - BUN 45
Considerations
Based on the above, his presentation is most concerning at this time for UGIB (upper gastrointestinal bleeding). Other things to consider on the differential, though are less likely, include Mallory-Weiss tear, LGIB (lower gastrointestinal bleeding).
Rockall score for UGIB (pre-endoscopy) is 4 points (1 for age, 0 for shock, 3 for liver failure), corresponding to a 24.6% mortality prior to endoscopy. Glasgow-Blatchford bleeding score is 12 points with the above values entered, making this “high risk” and a score above 6, associated with >50% risk of needing intervention.
Beyond using scores to help us risk stratify patients in the ED, ultrasound may also be able to augment our ability to determine whether our patients with GIB require more urgent/emergent intervention or may be medically managed in either inpatient or outpatient settings.
The Study
Results of a Prospective Study to Evaluate the Impact of Point-of-Care Ultrasound in the Enhancement of Gastrointestinal Bleeding Risk Scores
Chen et al recently undertook a study to evaluate the hemodynamic status of stable GI bleed patients using several ultrasound measures of volume status including collapsibility index of the IVC (inferior vena cava), systolic obliteration of the LV (left ventricle), LV outflow tract VTI (velocity time integral) pre and post-passive leg raise (1).
Criteria
Inclusion - GI bleeding in last 24 hrs, 18+ yo
Exclusion - previous ischemic arterial disease (TIA/stroke, peripheral arterial disease, coronary disease) in last 3 months, previous trauma/surgery with blood loss, pregnancy, and hemodynamic instability requiring admission to ICU (intensive care unit)
Examination
All studies performed by EM physician with long-standing experience in POCUS, as defined in article within 30 minutes of fluid resuscitation.
Collapsibility index of IVC
Visualize IVC in subxiphoid view, use M mode to measure IVC in both inspiration and expiration, compare
IVC diameter <2 cm with collapsibility of >=50% with each breath or collapsibility >=12% (calculated as max-min/mean x 100; all values are diameters)
If any of the above two criteria are met, suggests volume down and will be responsive to volume resuscitation
Systolic Obliteration of the Left Ventricle
Seen in image below, the walls of the LV touch, suggesting that the patient is volume down and will be responsive to volume resuscitation.
Image source https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201309-293OT
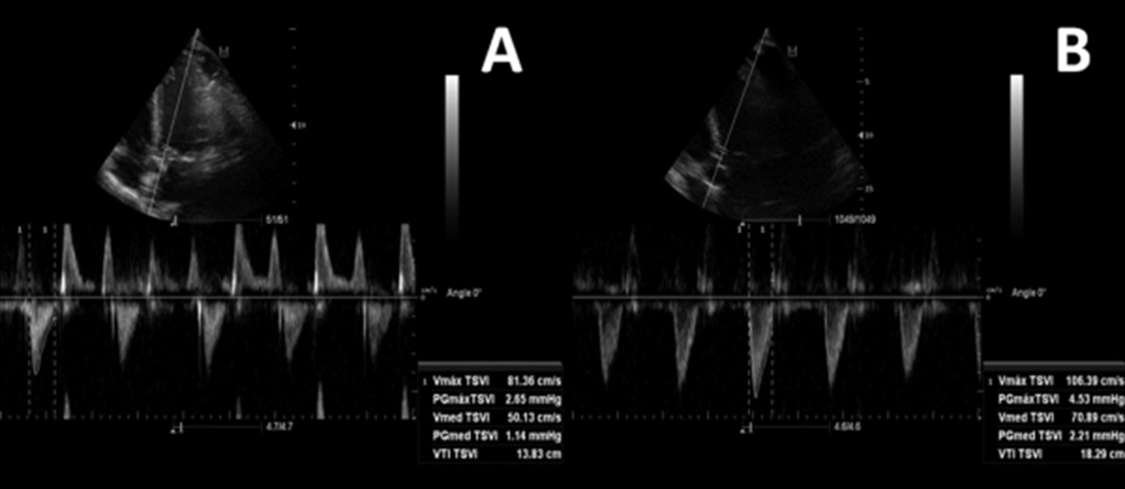
Left Ventricular Outflow Tract Velocity Time Integral
Identify the LVOT and measure the Vmed TSVi (velocity time integral) both pre and post-leg raise. A change of >=12.5% indicated likely volume down and likely will be responsive to volume resuscitation.
Image source https://onlinelibrary.wiley.com/doi/full/10.7863/ultra.15.14.08059
Performing these three ultrasound studies on 203 patients that met both inclusion and exclusion criteria, Chen et al found in UGIB patients, LV kissing walls were more commonly associated with adverse events (OR 3.8, 95% CI 1.32-10.96, P=0.01). They also noted that LGIB patients with IV collapsibility index of greater than 50% after passive leg raise also had more early adverse events (OR 3.6, 95% CI 1.45-9.00, P=0.004). Ultrasound was noted in the study to enhance sensitivity and specificity for both Rockall and Glasgow-Blatchford scores for late adverse events.
Conclusion/Take Home Points
Ultrasound may prove to be a useful tool in helping risk stratify patients with GIB beyond the available scoring systems.
Use the IVC collapsibility index, LV systolic obliteration (“kissing walls”), and LVOT VTI before and after passive leg raise to assess your patients.
References
Tung Chen, Y., Blancas Gómez‐Casero, R., Quintana Díaz, M., Villén Villegas, T., Cobo Mora, J. and Carballo Cardona, C., 2020. Results of a Prospective Study to Evaluate the Impact of Point‐of‐Care Ultrasound in the Enhancement of Gastrointestinal Bleeding Risk Scores. Journal of Ultrasound in Medicine, 39(2), pp.279-287.