"SO PAppy" - SOnographic Pediatric Appendicitis
Case: 12 year old boy coming in with his mother to your pediatric ED complaining of abdominal pain. He reports that the pain started around his belly button but moved to the lower right side. He developed a fever yesterday, and said when he tried to play basketball at school every time he jumped he felt a lot of pain in his stomach. You happen to have an ultrasound right next to you at bedside.
To start get the linear probe and have the curvilinear probe as back up and have the patient lie in a supine position. The linear probe has a higher frequency so the images will be especially clear on pediatric patients with smaller habitus.
Ask the patient to point with one finger where the pain is the worst, or alternatively place the probe at the site of maximal tenderness in the RLQ. i You want to capture images in both transverse and longitudinal views, but I prefer to start with transverse to identify more structures to get your bearings.
ii
iii
iv
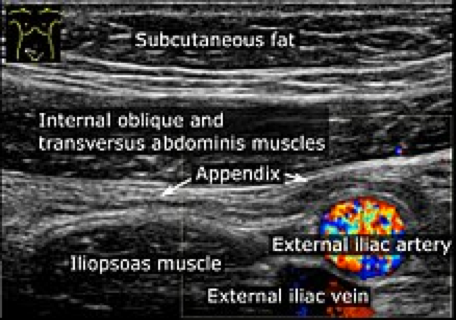
If you are lucky once you put the probe down at the site of maximal tenderness/pain you will see this…
v
Unfortunately most people will not get this view their first time and will have to use “graded compression”, which is just pushing gently on the abdomen to get rid of bowel gas to find key structures so you know where you are. To find the appendix it helps to first identify the iliac vessels, the psoas muscle, and the appendix usually lies on top or near the iliac vessels.
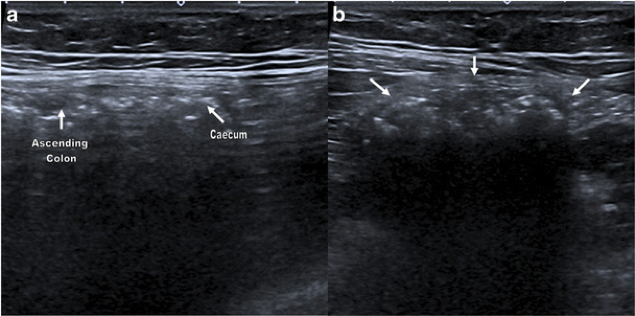
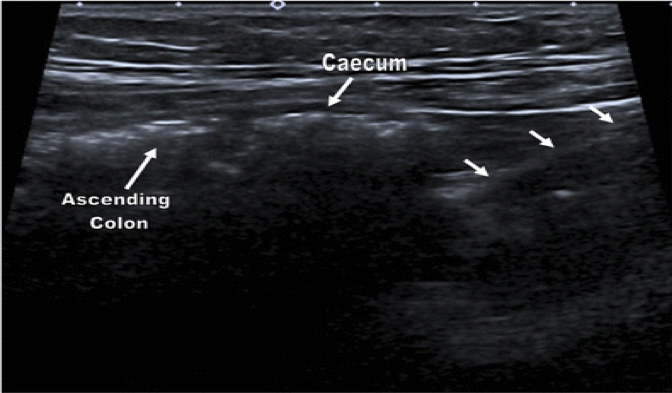
If the patient is too young to point where the pain is the worst, or you can’t identify the appendix with the above technique Sivitz et al described another technique with a sensitivity of 85% (95% confidence interval [CI] 75% to 95%), specificity of 93% (95% CI 85% to 100%), positive likelihood ratio of 11.7 (95% CI 6.9 to 20), and negative likelihood ratio of 0.17 (95% CI 0.1 to 0.28)vi. As seen to the right:
1-2) Move the probe laterally until you identify abdominal wall and ascending colon
3) Move down lateral border until you see cecum (a (long view),b (TV view) with small white arrows being cecum)
4) Move medially until you see psoas and iliac vessels (C)
5) With the psoas muscle and iliac vessels kept in view, move the transducer down into the pelvis and toward the umbilicus at the border of the cecum (D) red line) If the appendix is not yet visualized, place the probe in the sagittal position, identify the cecum in the long axis and sweep medially compressing the cecum against the psoas muscle
Hopefully, you'll see similar images to those below.
vii
ix
Hopefully, you have now found the appendix which is a blind-ended tubular structure that lacks peristalsis and can be traced back to the cecum. The 3 hard signs of diagnosing appendicitis are:
1) Non-compressibility
2) Diameter dilation greater than 6mm
3) Appendicolith (hyperechoic appendicolith within the lumen may be seen with posterior shadowing)
There are also secondary signs of appendicitis such as increased vascularity of the appendiceal wall may be appreciated as hyperemia with color flow Doppler, often referred to as the “ring of fire” on short axis. Finally, periappendiceal fluid collections may be seen suggesting edema or perforationx
xi
xii
In the end we were able to identify the appendix, measured the diameter to be 1.2cm, noncompressible, with an appendecolith and the patient was taken to the OR.
Imaging modalities:
US sensitivity is 98% and specificity is 92%
CT sensitivity is 94-100% and specificity is 93-100%
MRI sensitivity is 96% and specificity is 96% xiii
Author: Ari Nutovitz MD
Editor: Jeffery Greco MD
References:
[i] http://www.impocus.ca/knbology-and-machinery---transducer--
[ii] http://www.thepocusatlas.com/new-blog/appendicitis
[iv] https://epmonthly.com/impmedia/2012/12/Appy-long---labelled.jpg
[v] https://en.wikipedia.org/wiki/Appendix_(anatomy)
[vi] https://www.ncbi.nlm.nih.gov/pubmed/24882665
[vii] https://onlinelibrary.wiley.com/doi/pdf/10.1111/acem.13169
[viii] http://www.thepocusatlas.com/new-blog/appendicitis
[ix] https://link.springer.com/article/10.1007/s13244-013-0275-3
[xii] https://www.kkh.com.sg/news/patient-care/ultrasound-a-safer-way-to-diagnose-appendicitis-in-childre