Maisonneuve Fracture
Written By: Kirandeep Kaur, MD; Edited by: Timothy Khowong, MD, MSEd
What am I?
I twist and turn with a hidden sign,
A break that’s high, but seems just fine.
The ankle’s swollen, pain in the air,
But it’s not just a sprain—so beware!
I hide a tear where bones should meet,
And sometimes a bump on the ankle’s feat.
You might miss me with a quick glance,
But I’ll cause trouble if given the chance.
Case Presentation:
23 - year old male with no past medical history presented with a right leg splint after a fall while playing ice hockey. The tip of the ice skate got stuck in the ice causing him to invert his ankle and fall. He was unable to ambulate after the fall and EMS on the scene immobilized the knee and ankle. He is complaining of pain in his whole leg, but worse in his ankle
On exam, the patient had diffuse right ankle tenderness. No tenderness at the fibular head. Soft compartments, pulses, and sensation intact. Motor strength exam limited by pain, however able to range all toes
What Do You See:
Image A, B, C: Right Ankle XR (Obl, Lat, AP)
Impression: Acute, comminuted, mildly displaced fracture of the mid fibular diaphysis. Marked widening of the medial ankle joint space compatible with syndesmotic ligamentous injury. Talar dome appears intact.
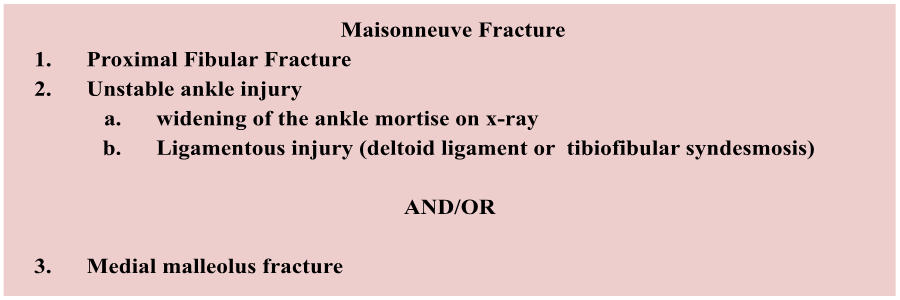
What Was It?
This patient had a Maisonneuve fracture, a serious injury. The classic mechanism of injury is an external rotational force to the foot, which typically occurs during activities like sports, or more commonly, in motor vehicle accidents or falls.
*Many times we anchor on the most obvious deformity in the imaging. It is important to review imaging in a systematic way in order to not miss other pathologies
Image D: TCS = tibiofibular clear space; TFO = tibiofibular overlap
The tibiofibular clear space should be no greater than 5mm, and the tibiofibular overlap should be no less than 1mm; otherwise, there is concern for the widening of the tibiofibular syndesmosis.The syndesmosis is a fibrous joint that holds the tibia and fibula together. When the joint is torn or disrupted, the medial malleolus can also be fractured. This cascade of injuries can lead to ankle instability, which, if untreated, can result in chronic pain and long-term joint problems.
Here are the Tib-Fib x-rays for the patient:
Image E, F, G: Right Tibia-Fibula x-ray (Lateral with ankle, lateral with knee, AP)
Treatment:
Most require surgical management
Fixation of the distal tibiofibular syndesmosis
Reduction and stabilization of the fibular fracture
fracture involving distal 2/3 of the fibula may compromise ankle mortise, and so may benefit from surgery
fracture involving proximal 1/3 fibula often managed non-operatively
Reduction and stabilization of medial malleolus fracture
Orthopedic Post-Op Instructions: Remove splint and work on range of motion in 2 weeks after surgery, but hold off on weight-bearing for 6-7 weeks.
Image H: Fluoroscopy from the OR post-operatively