Ortho Case: More Than Just A Shoulder Dislocation
Author: Kenneth Chang, DO
Peer-reviewer and Editor: Victor Huang, MD, CAQ-SM
Case: 80-year-old female presents to the Emergency Department with right shoulder pain after falling down half a flight of stairs. The patient denies any syncope, head injury, loss of consciousness, or neck pain. Vital signs are all in normal range. Physical examination shows decreased range of motion of the right shoulder, swelling and tenderness over the proximal humerus, and neurovascularly intact.
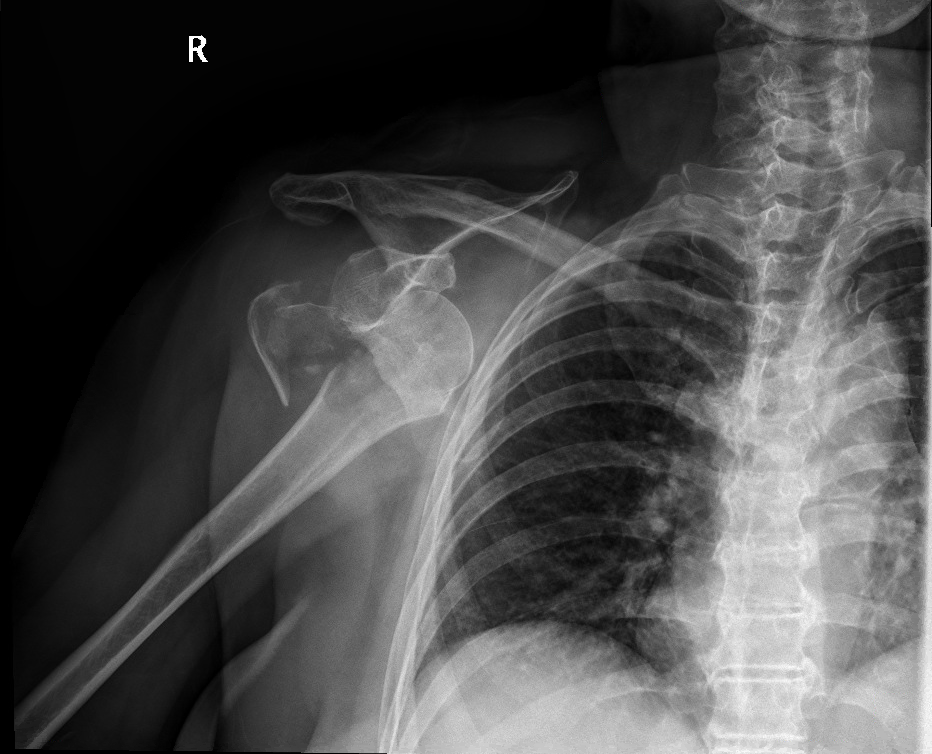
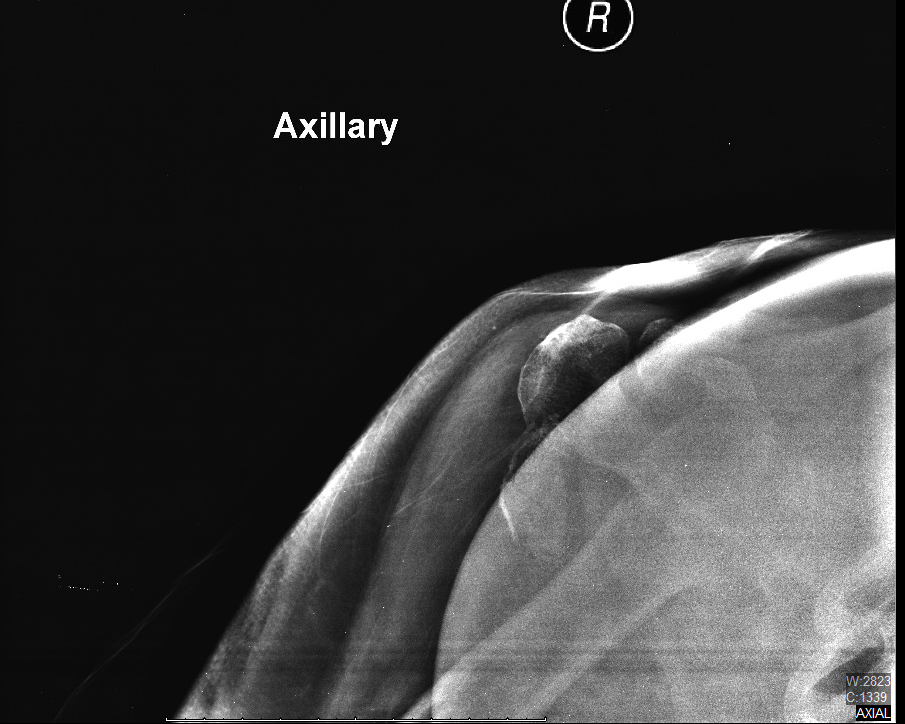
Figure 1. Image prompt. AP, scapular Y, and axillary views of the right shoulder. Author’s own images.
What is the diagnosis?
What are the risk factors and mechanism of injury?
What physical exam findings are expected?
Which imaging modalities can be used?
What is the management in the ED?
When do you consult Orthopedics
What is the definitive management of this injury?
See below for answers!
1. What is the diagnosis?
*Anterior inferior dislocation of the right glenohumeral joint with comminuted and displaced fracture of the greater tuberosity of the humerus*
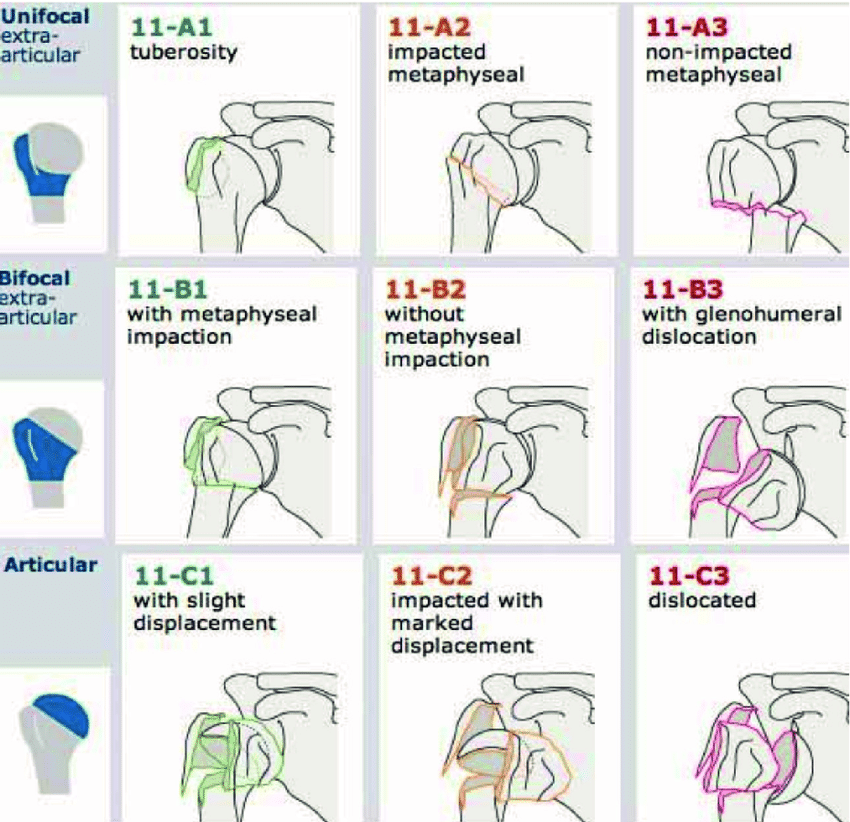
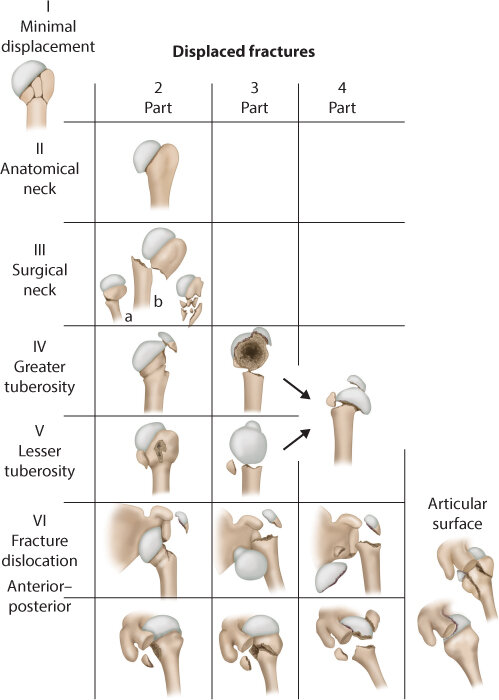
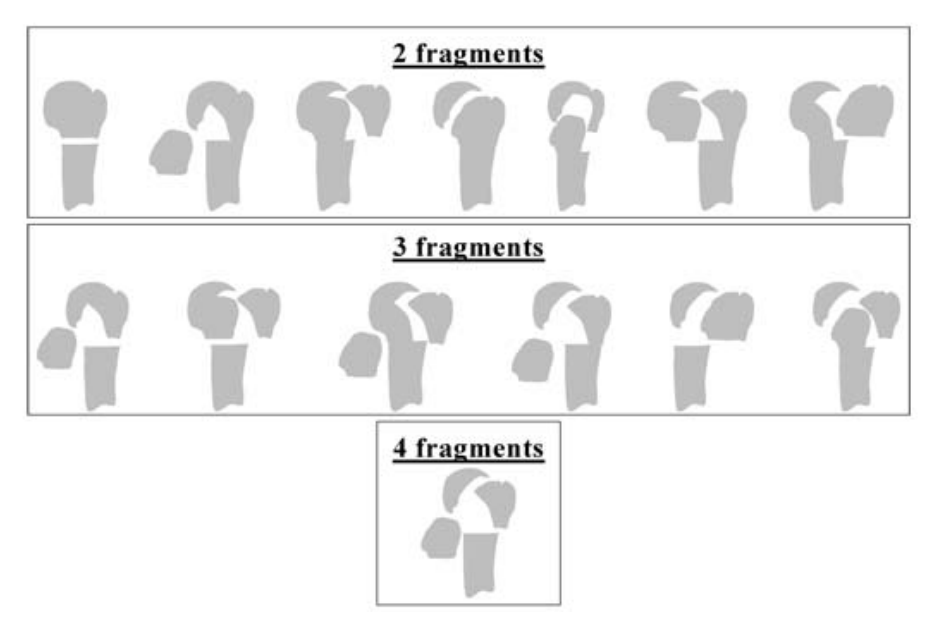
Pearl: Proximal humerus fracture dislocation can be classified based on the AO/OTA or Neer Classifications. The AO/OTA classification identifies 3 main fracture types with subgroups based on displacement, valgus or varus angulation of the humeral head, comminution, and presence and direction of glenohumeral joint dislocation. This scheme also places more emphasis on the integrity of the vascular supply to the articular surface, with increased risk of avascular necrosis from type A (low risk) to type C (high risk) [1]. Meanwhile, the Neer classification system divides the proximal humerus into 4 anatomical fracture segments: greater tuberosity, lesser tuberosity, humeral head (articular surface), and humeral shaft. Displacement is defined as > 1 cm or > 45 degrees of angulation [2].
These can further be classified as [2]:
One Part: non-displaced fracture, regardless of fragments from the fracture.
Two Part: one segment (not including the shaft) is displaced.
Three Part: displacement of one tuberosity plus the surgical neck
Four Part: all 4 segments displaced
Figure 2: Diagram of AO/OTA Classification
Figure 3: Diagram of Neer Classification [3].
2. What are the risk factors and mechanism of injury?
Proximal humerus fracture dislocations occur mostly due to low-energy mechanisms like ground level falls, often onto an outstretched hand [4]. Approximately 85% occur in patients > 50 years old, and are more common with osteoporotic bone [5]. In fact, proximal humerus fractures are the third most common fracture type in patients > 65 years old [2]. High-energy trauma is usually involved in younger individuals, which will often lead to other bone, soft tissue and neurovascular injuries [4].
3. What physical exam findings are expected?
A thorough physical exam should be performed to assess for concurrent injuries. Examination may show soft tissue swelling, ecchymosis, decreased convex contour of the shoulder and anterior of posterior bulging suggesting a dislocation. When performing the neurovascular exam, make sure to consider any signs of axillary nerve and artery injury. These signs may include decreased sensation on the lateral aspect of the proximal arm, decreased teres minor and deltoid motor function in the deltoid with external rotation and abduction of the shoulder. Axillary artery injuries are rare, but must be evaluated carefully with perfusion, capillary refill and distal pulses, as well as checking for ecchymosis, swelling and expanding hematomas in the axilla [6].
4. Which imaging modalities can be used?
Plain radiographs should be obtained with AP, scapular Y, and axillary views. Other considerations may include the Grashey (true AP) view to evaluate the glenohumeral joint articulation [7]. The Modified Velpeau view is similar to the axillary view, and is useful when the patient cannot abduct their arm.
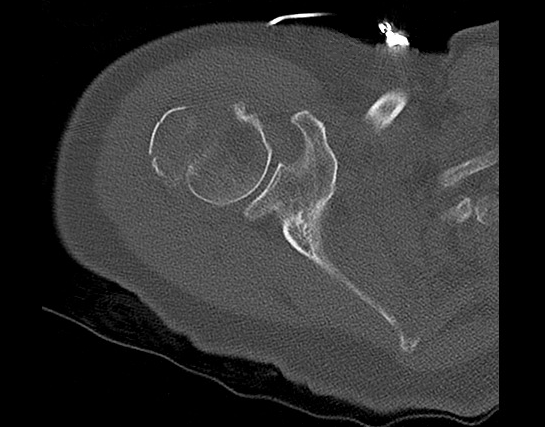
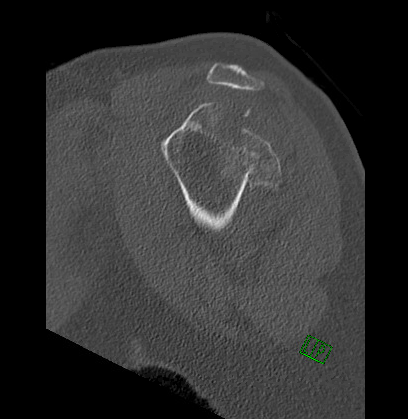
CT scans may be obtained for operative planning, assessment of intra-articular comminution, displacement of lesser or greater tuberosity fragments, and subtle coracoid fractures [7]. It provides a more precise view of the glenohumeral joint articulation when plain films are equivocal.
Figure 4: CT images of the right shoulder that demonstrate a comminuted and displaced fracture of the proximal humerus with a reduced glenohumeral joint. Author’s own images.
5. What is the management in the ED?
In the ED, the management of the anterior shoulder dislocation with isolated greater tuberosity fracture includes urgent reduction under procedural sedation. In a 2017 European retrospective cohort study, standard ED reduction with sedation and manipulation with the modified Hippocratic technique was successful in up to 94% of these injuries, and there was no further propagation of the fracture. It is reasonable to attempt reduction for a two part fracture dislocation with an isolated greater tuberosity fracture [8].
Figure 5. Post-reduction images that demonstrate interval reduction of the glenohumeral joint and displaced fracture of the greater tuberosity again seen. Author’s own images.
6. When do you consult Orthopedics?
Orthopedics should be consulted when there is a complicated reduction, irreducible dislocation, neurovascular compromise, multiple fracture fragments, open fractures, or when expedited surgical intervention is indicated. Anterior dislocation with a surgical neck fracture and posterior dislocations with any fracture type may be better managed under general anesthesia in the OR [8]. Involvement of the humeral shaft, glenoid rim or larger greater tuberosity fragments are associated with higher risk of iatrogenic injury during reduction [9]. Three or four part fracture dislocations should be managed with Orthopedics because these are rare, complex and associated with devascularization of the humeral head [10,11].
7. What is the definitive management of this injury?
Non-operative injuries should be immobilized in a sling and be closely followed with outpatient Orthopedics. These patients should undergo physical therapy as soon as possible for quicker recovery. A complication of an anterior shoulder dislocation with a greater tubercle fracture is decreased range of motion, but this is thought to reduce joint instability which leads to lower rates of recurrent dislocations [12].
Operative injuries are less common. Numerous factors including age, fracture type, bone quality, comorbidities, and concurrent injuries are used to determine the optimal type of surgical intervention. In two part fractures, one surgical indication is based on the degree of displacement (GT displacement < 5mm are nonoperative and > 5mm are operative). The greater the degree of displacement, the greater risk of functional impairment with decreased range of motion (especially external rotation and abduction) without any surgical intervention [12]. For younger patients, ORIF is preferred and has optimal functional outcomes. Isolated screw fixation may also be used in younger patients with normal bone structure. In older patients with osteoporosis, non-absorbable sutures are used and hardware is avoided due to risk of impingement. In these cases, the preferred surgical management may include reverse shoulder arthroplasty (RSA) or hemiarthroplasty, both of which would have less of a detrimental effect on weak osteopoerotic bone [10,11].
Works Cited
Marongiu, G., Leinardi, L., Congia, S. et al. Reliability and reproducibility of the new AO/OTA 2018 classification system for proximal humeral fractures: a comparison of three different classification systems. J Orthop Traumatol 21, 4 (2020). https://doi.org/10.1186/s10195-020-0543-1
Carofino BC, Leopold SS. Classifications in brief: the Neer classification for proximal humerus fractures. Clin Orthop Relat Res. 2013;471(1):39-43. doi:10.1007/s11999-012-2454-9
Mora Guix JM, Pedrós JS, Serrano AC. Updated classification system for proximal humeral fractures. Clin Med Res. 2009;7(1-2):32-44. doi:10.3121/cmr.2009.779
Flint JH, Carlyle LM, Christiansen CC, Nepola J V. Case report and literature review anterior shoulder dislocation with three-part proximal humerus fracture and humeral shaft fracture. Iowa Orthop J. 2009;29:105-113. Accessed August 12, 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/19742096/?tool=EBI
Court-Brown CM, McQueen MM. Two-part fractures and fracture dislocations. Hand Clin. 2007 Nov;23(4):397-414, v. doi: 10.1016/j.hcl.2007.08.003. PMID: 18054667
Venkatesh Palanisamy J, Vaithilingam A, Das S, Trikha V. Proximal humerus fracture dislocation leading to axillary artery injury in an young adult: Case report of an unusual presentation. Published online 2017. doi:10.1016/j.jcot.2017.05.006
Plachel F, Schanda JE, Ortmaier R, Auffarth A, Resch H, Bogner R. The "triple dislocation fracture": anterior shoulder dislocation with concomitant fracture of the glenoid rim, greater tuberosity and coracoid process-a series of six cases. J Shoulder Elbow Surg. 2017 Sep;26(9):e278-e285. doi: 10.1016/j.jse.2017.01.022. Epub 2017 Mar 31. PMID: 28372969
Wronka KS, Ved A, Mohanty K. When is it safe to reduce fracture dislocation of shoulder under sedation? Proposed treatment algorithm. Eur J Orthop Surg Traumatol. 2017;27(3):335-340. doi:10.1007/s00590-016-1899-z
Guo J, Liu Y, Jin L, Yin Y, Hou Z, Zhang Y. Size of greater tuberosity fragment: a risk of iatrogenic injury during shoulder dislocation reduction. Int Orthop. 2019;43(5):1215-1222. doi:10.1007/s00264-018-4022-8
Robinson CM, Khan LA, Akhtar MA. Treatment of anterior fracture-dislocations of the proximal humerus by open reduction and internal fixation. J Bone Joint Surg Br. 2006 Apr;88(4):502-8. doi: 10.1302/0301-620X.88B4.17195. PMID: 16567786.
Schirren M, Siebenbürger G, Fleischhacker E, et al. Anterior fracture dislocation of the proximal humerus: Management and treatment results. Obere Extrem. 2019;14(2):103-109. doi:10.1007/s11678-019-0509-1
Dussing F, Plachel F, Grossauer T, et al. Anterior shoulder dislocation and concomitant fracture of the greater tuberosity: Clinical and radiological results. Obere Extrem. 2018;13(3):211-217. doi:10.1007/s11678-018-0451-7